Withdrawal Symptoms: What They Are, Why They Happen, and How to Handle Them
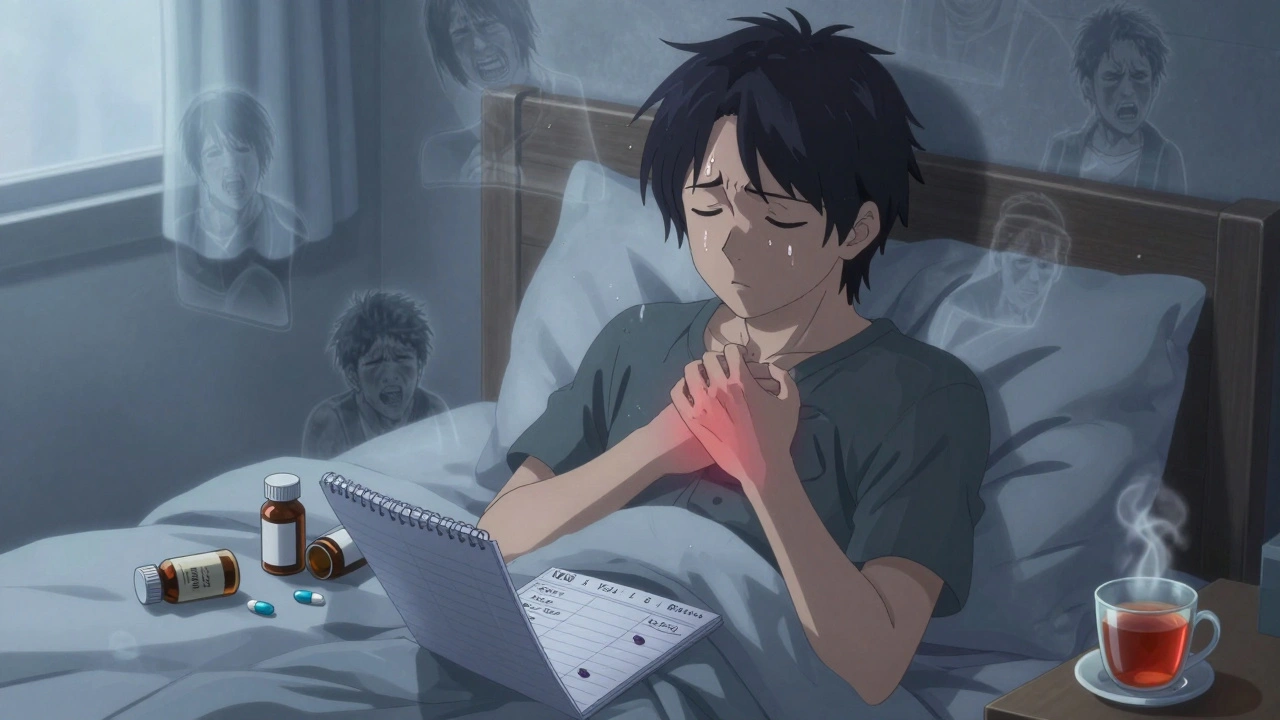
When your body gets used to a medication or substance and then suddenly doesn’t get it anymore, withdrawal symptoms, the physical and mental reactions that happen after stopping a regularly used substance. Also known as drug withdrawal, it’s not just "feeling off"—it’s your nervous system scrambling to readjust. This isn’t weakness. It’s biology. Whether you’re on a prescription drug like an antidepressant, a painkiller like opioids, or even something like caffeine, your brain has adapted. And when the supply drops, it doesn’t know how to cope—fast.
Some opioid withdrawal, the set of physical and emotional reactions after stopping opioids like oxycodone or fentanyl. Also known as narcotic withdrawal, it can include nausea, muscle aches, sweating, and intense anxiety. Others might experience antidepressant discontinuation, the range of symptoms like dizziness, brain zaps, and mood swings after stopping SSRIs or SNRIs. Also known as SSRI withdrawal, it’s often mistaken for a relapse of depression. Even antibiotics like linezolid or common painkillers can cause reactions if stopped abruptly. These aren’t random side effects—they’re your body’s signal that it’s been depending on something to function normally.
What makes withdrawal tricky is how unpredictable it can be. Two people stopping the same drug at the same dose might have totally different experiences. One might feel tired for a few days. Another could end up in the ER. That’s why timing matters. Tapering slowly under medical supervision isn’t optional—it’s the safest path. And it’s not just about the drug. Your health, age, how long you’ve been taking it, and even your stress levels all play a role.
You’ll find posts here that dig into real cases: how trimethoprim can mess with your potassium and cause symptoms that feel like withdrawal, why stopping SGLT2 inhibitors suddenly might trigger ketoacidosis, and how even something as simple as kava or turmeric can cause rebound anxiety if you quit cold turkey. These aren’t just drug facts—they’re survival guides for people trying to get off something they’ve relied on.
There’s no one-size-fits-all fix. But knowing what to expect, what to watch for, and when to call your doctor can make all the difference. The posts below give you the straight talk you won’t get from a pharmacy flyer: what the science says, what patients actually experience, and how to protect yourself when you’re trying to move on from a medication that changed your life—whether for better or worse.
Opioid Withdrawal: How to Safely Taper and Manage Symptoms
Learn how to safely taper off opioids with a step-by-step guide to managing withdrawal symptoms, using medications, and building long-term recovery. Based on CDC guidelines and real patient outcomes.
learn more