Stopping opioids after long-term use isn’t just a matter of quitting cold turkey. It’s a physical and emotional process that can go badly if done too fast. Many people don’t realize that even prescribed opioids can create dependence. When you’ve been taking them for weeks or months, your body adapts. Suddenly cutting off the supply triggers a cascade of symptoms that can feel like the flu on steroids - plus anxiety, insomnia, and crushing cravings. The good news? You don’t have to suffer through it alone. With the right plan, tapering can be done safely, with manageable symptoms and real progress.
Why Tapering Matters
Rapid opioid withdrawal isn’t just uncomfortable - it’s dangerous. A 2017 study published in Pain Medicine found that people forced to stop opioids too quickly were 3.5 times more likely to have suicidal thoughts. Emergency room visits for withdrawal symptoms jumped by 41% in patients who underwent fast tapers, according to Oregon Health Authority data from 2020. The CDC’s 2022 guidelines make this clear: if your current opioid dose isn’t putting you in immediate danger, there’s no rush to stop. Tapering should be about safety, not speed.People often start tapering for good reasons - pain improved after surgery, side effects like constipation or drowsiness became unbearable, or they noticed they were using more than prescribed. But the biggest driver? Fear. Fear of addiction. Fear of overdose. Fear that doctors will cut them off. That fear leads to rushed decisions. And rushed decisions lead to suffering.
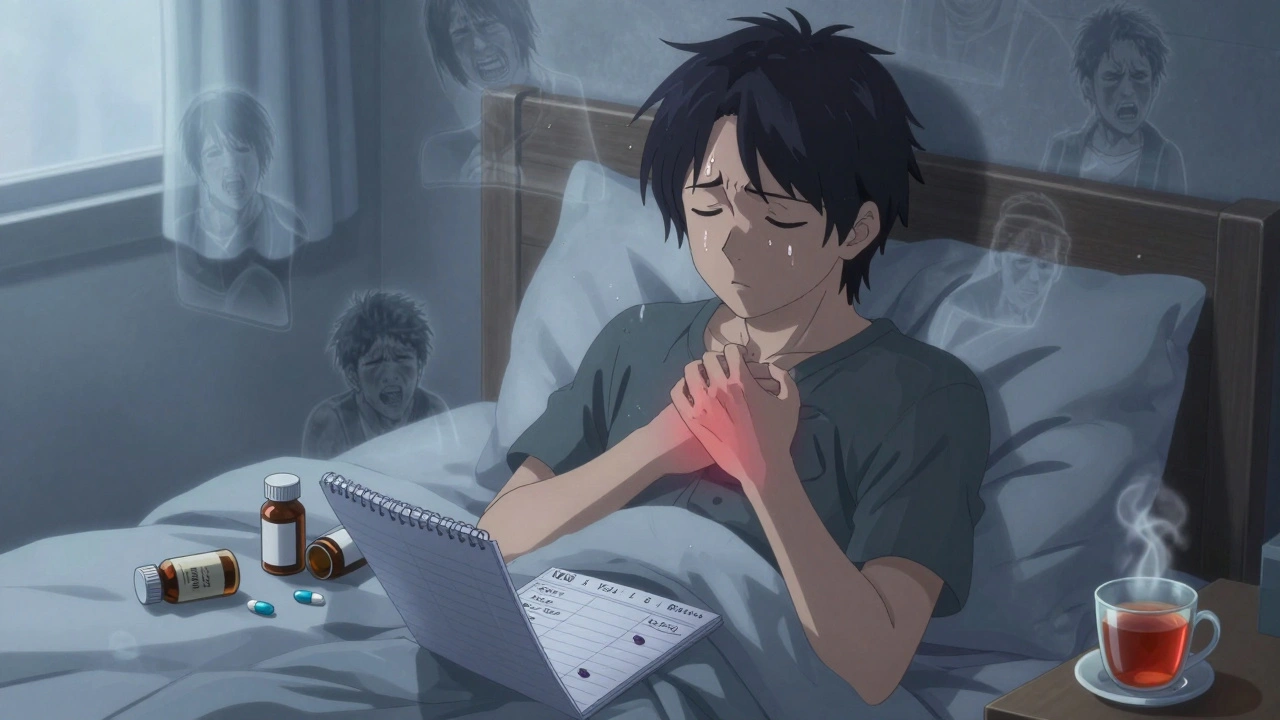
What Happens During Withdrawal?
Withdrawal symptoms start within hours of your last dose and peak around days 2-4. They’re not the same for everyone, but here’s what most people experience:- Nausea (87% of cases)
- Muscle aches (85%)
- Anxiety (80%)
- Insomnia (78%)
- Diarrhea (75%)
- Sweating, chills, runny nose
- Strong cravings
These aren’t just "in your head." They’re real, measurable physiological reactions. Your nervous system has been trained to rely on opioids to feel normal. When you remove them, it goes into overdrive. That’s why symptoms feel so intense. The DSM-5, the standard diagnostic manual used by clinicians, lists these as hallmark signs of opioid withdrawal.
Some people worry about long-term effects. The truth? Most physical symptoms fade within 7-10 days. But psychological ones - anxiety, low mood, trouble sleeping - can linger for weeks. That’s why tapering isn’t just about reducing pills. It’s about preparing your body and mind for life without them.
How Fast Should You Taper?
There’s no one-size-fits-all taper. Speed depends on how long you’ve been on opioids, your dose, your health, and your mental state. Here’s what the evidence says:- Fast taper: Reducing by 20-25% every few days. This is risky. A 2018 JAMA Internal Medicine study showed 68% higher rates of severe symptoms and a 5.2 times higher dropout rate.
- Slow taper: Reducing by 5-10% every 2-4 weeks. This is the gold standard. A 2020 Oregon study found 73% better adherence and far fewer ER visits.
- Very slow taper: For people on high doses (over 90 mg morphine equivalent daily dose) or those who’ve been on opioids for years, tapers can last 6 months to 2 years. The VA recommends this for long-term users.
For example, someone taking 8 pills a day might drop one pill every 3-4 days. That’s a 12.5% reduction per step. By day 14, they’re down to one pill daily. Then they hold for a week before cutting again. This pace gives the body time to adjust without triggering major withdrawal.
Don’t let insurers or clinics push you into a 30-day plan if you’ve been on opioids for 5 years. That’s not care - that’s cost-cutting. Your taper should be as long as it needs to be.
Medications That Help
You don’t have to power through withdrawal alone. Several FDA-approved and off-label medications can ease symptoms:- Lofexidine (Lucemyra): Approved in 2018 and expanded in 2024 to an extended-release form, this non-opioid drug reduces anxiety, sweating, and muscle aches by calming the nervous system. It doesn’t block cravings, but it makes the process bearable.
- Gabapentin: Often used for nerve pain, it helps with anxiety, insomnia, and restlessness. Start at 100-300 mg, build up to 1,800-2,100 mg per day in divided doses. Many patients report better sleep within days.
- Baclofen: A muscle relaxant that reduces cravings and physical discomfort. Typical dose: 5 mg three times daily, increased slowly to 40 mg daily.
- Clonidine: Sometimes used off-label to reduce sweating, anxiety, and high blood pressure during withdrawal. Requires careful monitoring.
These aren’t magic pills. They’re tools. Used right, they can turn a nightmare into a tough but manageable process. Always work with a doctor to find the right combination and dose.
What to Avoid
Some strategies sound helpful but make things worse:- Going cold turkey: Especially on high doses, this can trigger seizures, extreme dehydration, or cardiac stress.
- Using alcohol or benzodiazepines to self-medicate: This adds another dependency and increases overdose risk.
- Switching to another opioid: Like switching from oxycodone to heroin or fentanyl. This doesn’t solve the problem - it just changes the drug.
- Ignoring mental health: Depression and anxiety often worsen during withdrawal. If you’re feeling hopeless, talk to someone. Therapy isn’t optional - it’s essential.
Also avoid doctors who refuse to adjust your plan. If you’re having severe symptoms, your taper should slow down - not speed up. A good provider listens. A bad one follows a script.
Support Beyond Pills
Medications help with the body. But your mind needs help too. Research shows people who combine tapering with behavioral support have much better outcomes:- Cognitive Behavioral Therapy (CBT): Used by 41% of successful taperers, CBT helps reframe thoughts about pain and cravings. It teaches you to ride out urges without acting on them.
- Acupuncture: Reported as helpful by 33% of patients in Oregon’s 2021 registry. It doesn’t cure withdrawal, but many report less muscle pain and better sleep.
- Physical therapy: If chronic pain led to inactivity, PT helps rebuild strength and mobility without opioids.
- Support groups: Reddit’s r/OpiatesRecovery has over 145,000 members. People share real stories - like one user who tapered from 120 mg morphine daily over 6 months using 10% monthly cuts. Symptoms were mild: slight insomnia, low energy. No ER visits.
One patient on Healthgrades wrote about being forced to drop from 180 mg MEDD to zero in 4 weeks. She ended up in the ER with vomiting, shaking, and panic attacks. She needed hospitalization. That’s what happens when tapering isn’t personalized.

How to Know If Your Taper Is Working
Progress isn’t just about reducing pills. It’s about your quality of life:- Are you sleeping better?
- Are you moving more - walking, stretching, doing chores?
- Are you spending time with family instead of isolating?
- Is your anxiety less intense?
- Do you feel more in control?
Track these. Write them down. If your pain is still high but you’re not using opioids to cope, that’s progress. If you’re sleeping 6 hours instead of 2, that’s progress. If you went a week without a craving, that’s huge.
The CDC recommends checking in with your provider every 2-4 weeks. Bring your notes. Ask: "Is this pace right for me?" If you’re struggling, say so. A good plan bends to your needs.
What Comes After Tapering?
Stopping opioids isn’t the finish line. It’s the start of a new phase: living without them. Many people think, "Now I’m clean, I’m fine." But pain doesn’t vanish. Neither does anxiety.This is where non-opioid pain management kicks in:
- Exercise (even walking 20 minutes a day)
- Heat therapy, massage, or TENS units
- Mindfulness and breathing techniques
- Working with a pain psychologist
Academic medical centers are now offering coordinated care - combining physical therapy, counseling, and medication management. That’s the future. And it works. A 2022 American Pain Society survey found 67% of centers now offer these full programs.
Long-term, people who complete slow tapers with support report better function, less depression, and improved sleep. A 2020 survey showed 78% felt more in control of their lives. That’s the real win.
Final Thoughts
Opioid tapering isn’t about punishment. It’s about reclaiming your health. You didn’t fail by becoming dependent. You were prescribed a tool that worked - and then kept working. Now it’s time to move on.Slow is safe. Slow is sustainable. Slow is what saves lives. If your doctor pushes you to go faster than you’re ready for, ask for a second opinion. You have the right to a plan that respects your body, your pain, and your pace.
There’s life after opioids. It’s not perfect. It’s not easy. But it’s yours - and it’s worth fighting for.
How long does opioid withdrawal last?
Physical symptoms like nausea, muscle aches, and diarrhea usually peak within 72 hours and fade within 7-10 days. But psychological symptoms - anxiety, trouble sleeping, low mood - can last for weeks or even months. That’s why slow tapering and ongoing support are critical. The body recovers faster than the mind, and both need time.
Can you taper off opioids at home?
Yes, many people do - but only under medical supervision. You need a doctor to create a tapering schedule, monitor your symptoms, and adjust your plan. Self-tapering without support increases the risk of relapse, severe withdrawal, or overdose. If you’re on a high dose or have mental health conditions, inpatient or outpatient support is strongly recommended.
What if my pain gets worse during tapering?
Breakthrough pain is common during tapering - affecting nearly 70% of patients. Don’t panic. Talk to your provider. They may adjust your taper speed, add non-opioid pain meds like gabapentin or NSAIDs, or recommend physical therapy. Stopping the taper isn’t failure. It’s part of the process. The goal isn’t to eliminate pain completely - it’s to manage it without opioids.
Is it safe to use marijuana during opioid withdrawal?
Some people find cannabis helps with sleep, anxiety, and nausea during withdrawal. But there’s limited clinical evidence, and it’s not FDA-approved for this use. If you’re considering it, talk to your doctor. It can interact with other medications and may not be legal in your area. Don’t replace one dependency with another. Use it cautiously, if at all.
How do I know if I need professional help?
You need professional help if you’re on high-dose opioids (over 90 mg morphine equivalent daily), have a history of depression or suicidal thoughts, have other substance use issues, or feel overwhelmed by symptoms. If you’ve tried tapering before and relapsed, or if your doctor suggests it, don’t go it alone. Programs that combine medical care, therapy, and peer support offer the best chance for success.
Will I ever feel normal again?
Yes - but it takes time. Most people report feeling like themselves again within 3-6 months after completing a slow taper. Sleep improves. Energy returns. Mood stabilizes. The brain slowly resets. It’s not instant. But with patience and support, your body regains its natural balance. You don’t need opioids to feel okay.
For more information, refer to the CDC’s 2022 Clinical Practice Guideline for Prescribing Opioids for Pain and the HHS Guide for Clinicians on the Appropriate Dosage Reduction or Discontinuation of Long-Term Opioid Analgesics.
Taya Rtichsheva
December 7, 2025 AT 21:01Christian Landry
December 9, 2025 AT 17:54Philippa Barraclough
December 10, 2025 AT 13:55Tim Tinh
December 10, 2025 AT 16:57Katie Harrison
December 10, 2025 AT 20:04Mona Schmidt
December 12, 2025 AT 06:29Rich Paul
December 13, 2025 AT 07:57Chris Marel
December 13, 2025 AT 13:09Delaine Kiara
December 13, 2025 AT 17:59Nikhil Pattni
December 14, 2025 AT 00:01Ajit Kumar Singh
December 14, 2025 AT 23:36Lola Bchoudi
December 15, 2025 AT 09:22Guylaine Lapointe
December 16, 2025 AT 08:55Tiffany Sowby
December 18, 2025 AT 06:25