SGLT2 Inhibitors: What They Are, How They Work, and What You Need to Know
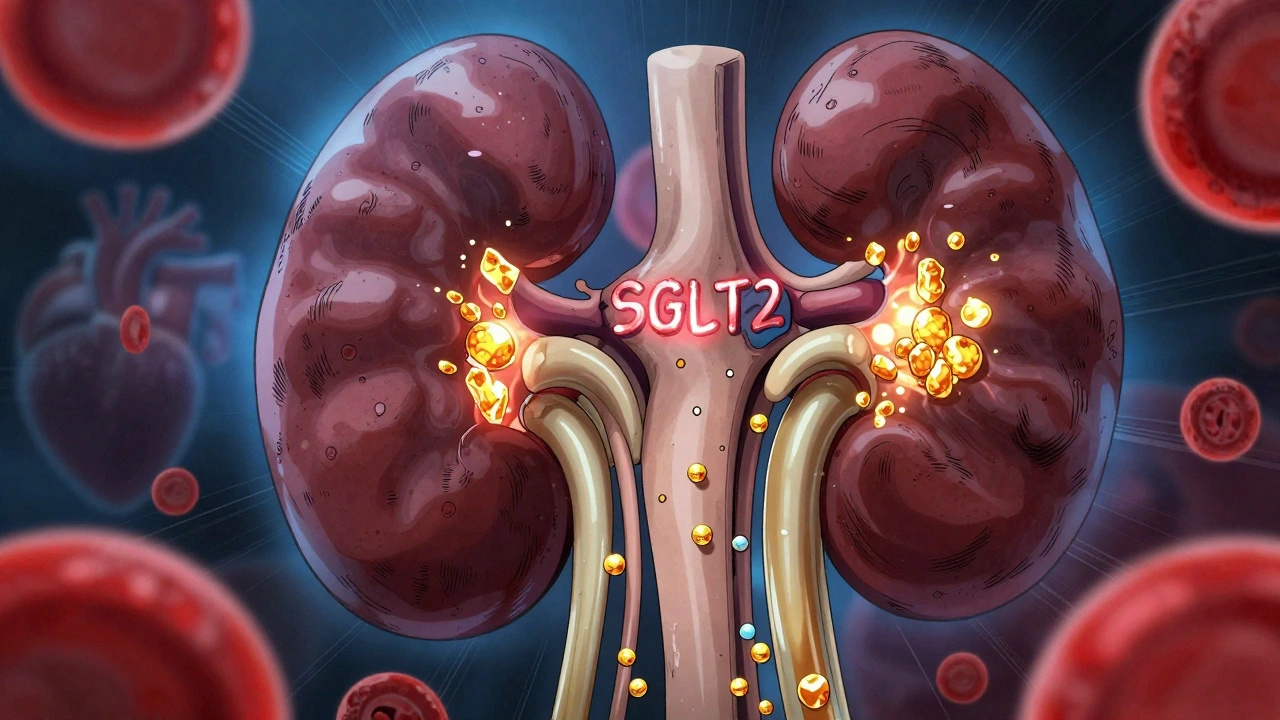
When you hear SGLT2 inhibitors, a class of prescription drugs used primarily to lower blood sugar in people with type 2 diabetes. Also known as gliflozins, they work by making your kidneys flush out extra sugar through urine—instead of reabsorbing it like they normally would. That’s it. No magic. No complex mechanisms. Just your body doing what it’s already designed to do, but now guided by medicine.
What makes these drugs different isn’t just how they lower blood sugar—it’s what else they do. SGLT2 inhibitors, including drugs like empagliflozin, dapagliflozin, and canagliflozin, have been shown in large studies to reduce the risk of heart failure hospitalizations and slow kidney disease progression—even in people without diabetes. That’s rare. Most diabetes drugs only focus on glucose. These go further. They don’t just treat a number; they protect organs.
And they’re not just for older adults with long-term diabetes. People with heart failure, even if they don’t have diabetes, are now prescribed these pills because they reduce fluid overload and improve heart function. Kidney protection, a key benefit of SGLT2 inhibitors, isn’t a side effect—it’s a core outcome. In fact, the FDA has approved them for use in chronic kidney disease, regardless of diabetes status. That’s a big deal. It means these drugs are being used for more than just blood sugar control.
But they’re not without trade-offs. Because they make you pee out sugar, you might get more yeast infections, especially in women. Dehydration and low blood pressure can happen if you’re not drinking enough water. And in rare cases, they can cause a serious condition called diabetic ketoacidosis—even when blood sugar looks normal. That’s why you need to know the signs: nausea, vomiting, stomach pain, confusion. Don’t ignore them.
These drugs work best when you’re already eating right, moving regularly, and taking other meds as prescribed. They’re not a replacement for lifestyle—they’re a tool that makes it easier to stay on track. Many people find they lose a few pounds on them, not because they’re dieting, but because they’re losing sugar calories through urine.
What you’ll find in the posts below aren’t just drug facts. You’ll see real stories about managing side effects, how these drugs interact with antibiotics like trimethoprim, why some people stop taking them after a safety alert, and how they fit into broader medication safety practices. You’ll learn how generic versions are tested for safety, how pharmacists handle substitutions, and what happens when you combine them with other drugs like blood thinners or NSAIDs. These aren’t theoretical discussions—they’re grounded in what patients actually experience, what studies show, and what the FDA monitors.
Whether you’re taking one of these drugs, considering it, or just trying to understand why your doctor recommended it, this collection gives you the practical, no-fluff details you need to make sense of it all. No jargon. No hype. Just what matters.
SGLT2 Inhibitors for Type 2 Diabetes: What You Need to Know About Benefits and Risks
SGLT2 inhibitors like Jardiance and Farxiga offer powerful heart and kidney protection for type 2 diabetes patients-but come with risks like yeast infections, ketoacidosis, and kidney stress. Know who benefits most and what to watch for.
learn more