When you’re managing type 2 diabetes, the goal isn’t just to lower your blood sugar-it’s to protect your heart, kidneys, and overall life expectancy. That’s where SGLT2 inhibitors come in. These aren’t your grandfather’s diabetes pills. Since the first one, canagliflozin, hit the market in 2013, this class of drugs has rewritten the rules for how we treat type 2 diabetes. They don’t just help with glucose. They save lives. But they also come with real, sometimes serious, side effects you can’t ignore.
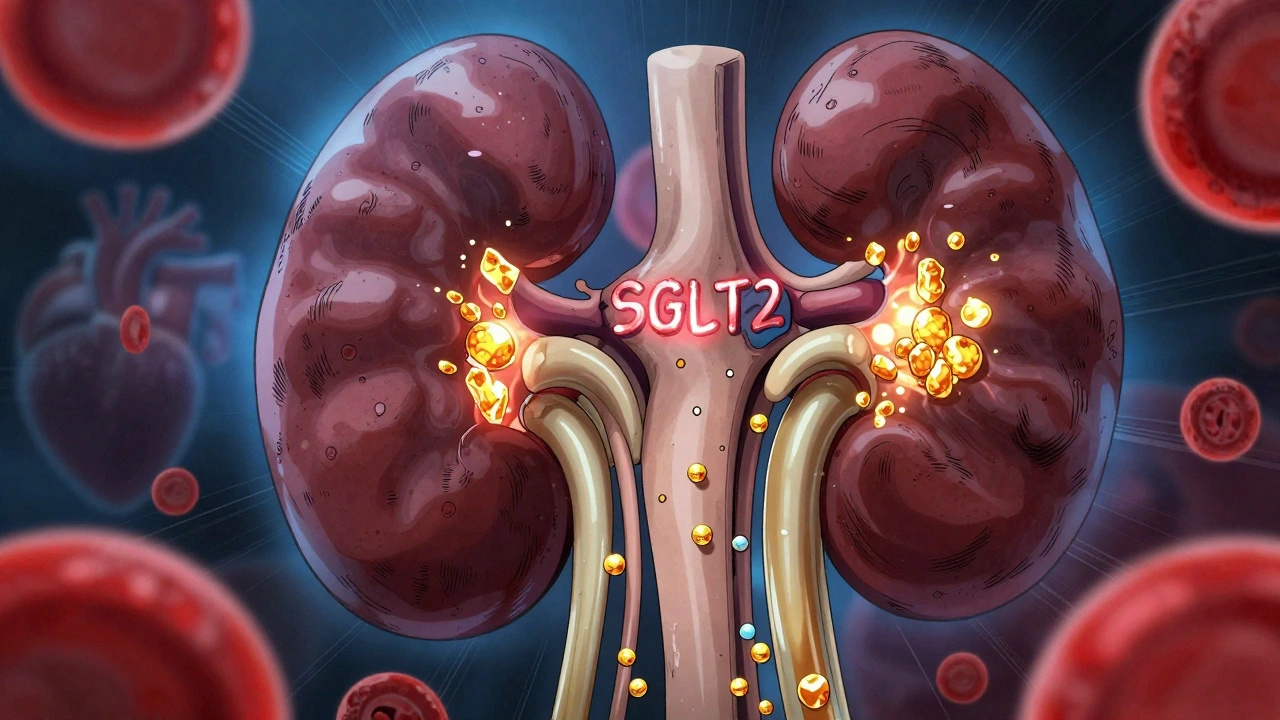
How SGLT2 Inhibitors Actually Work
Most diabetes medications push insulin around or make your body more sensitive to it. SGLT2 inhibitors do something completely different. They tell your kidneys to flush out extra sugar-literally. These drugs block a protein in your kidneys called SGLT2, which normally reabsorbs glucose back into your bloodstream. When it’s blocked, about 40 to 100 grams of glucose spill into your urine every day. That’s the equivalent of 10 to 25 teaspoons of sugar you’re peeing out.
This mechanism means you lose weight without trying-most people drop 2 to 3 kilograms in the first few months. Blood pressure drops too, usually by 3 to 5 mmHg. And because the drug works independently of insulin, your risk of low blood sugar is extremely low unless you’re also on insulin or sulfonylureas.
The four main SGLT2 inhibitors on the market are:
- Canagliflozin (Invokana)
- Dapagliflozin (Farxiga)
- Empagliflozin (Jardiance)
- Ertugliflozin (Steglatro)
All of them reduce HbA1c by about 0.6% to 0.8% as monotherapy. That’s solid, but not revolutionary-until you look at what else they do.
The Life-Saving Benefits You Won’t Find on a Glucometer
What made SGLT2 inhibitors a medical revolution wasn’t their glucose-lowering. It was what happened in big clinical trials.
The EMPA-REG OUTCOME trial, which followed over 7,000 people with type 2 diabetes and heart disease, found that empagliflozin reduced the risk of dying from heart problems by 38%. That’s not a small tweak-it’s a game-changer. The CANVAS Program showed similar results with canagliflozin: a 14% drop in heart attacks, strokes, or cardiovascular death.
But the real shocker came with heart failure. Before these drugs, we had few options to stop the downward spiral of heart failure in diabetics. Now, SGLT2 inhibitors cut hospitalizations for heart failure by 30% to 35%, even in people without diabetes. The DAPA-HF and EMPEROR-Preserved trials proved this across all types of heart failure-whether the heart was pumping weakly or just stiffening up.
And then there’s the kidneys. The CREDENCE trial showed canagliflozin reduced the risk of kidney failure, doubling of creatinine, or kidney-related death by 30%. The DAPA-CKD and EMPA-KIDNEY trials later confirmed this benefit even in people without diabetes. That’s why, in 2023, the American Diabetes Association upgraded SGLT2 inhibitors to first-line therapy for anyone with type 2 diabetes who has heart disease, heart failure, or chronic kidney disease-even before metformin.
These aren’t theoretical benefits. Real patients report them. One man in Sacramento saw his heart’s ejection fraction climb from 28% to 42% after switching to Jardiance. Another woman lost 15 pounds in three months without changing her diet. These aren’t outliers-they’re expected outcomes.
The Dark Side: Risks You Can’t Ignore
Nothing in medicine is free. For SGLT2 inhibitors, the cost comes in side effects.
The most common? Genital yeast infections. About 6% to 11% of women and 3% to 5% of men get them. It’s not a joke-it’s uncomfortable, recurrent, and sometimes leads to stopping the drug. Men can get balanitis; women, vulvovaginal candidiasis. Good hygiene helps, but if you’ve had frequent yeast infections before, this might not be the right drug for you.
Urinary tract infections (UTIs) are also more common, especially in women. About 6% to 9% of users get them, compared to 4% on placebo. Most are mild, but they can escalate. If you’re prone to UTIs, monitor closely.
Then there’s the scary one: diabetic ketoacidosis (DKA). But here’s the twist-it’s often euglycemic DKA. That means your blood sugar might only be 180 or 220 mg/dL, not 400+. You won’t feel the classic warning signs. You might just feel nauseous, tired, or short of breath. And it can happen even if you’re not sick. A 2022 study found 42% of these cases occurred in people with normal kidney function. The FDA requires a black box warning for this. If you’re scheduled for surgery, sick with the flu, or cutting carbs drastically, your doctor should tell you to pause your SGLT2 inhibitor.
Acute kidney injury is another risk. The FDA has logged over 1,800 reports since 2013. It’s rare-about 0.78 events per 1,000 patient-years-but it happens. Elderly patients, those on diuretics, or anyone dehydrated are at higher risk. That’s why doctors check your kidney function before starting and every few months after.
Canagliflozin has a specific risk: lower limb amputations. In the CANVAS trial, the rate was nearly double compared to placebo. It’s rare-about 1 in 100 people over 5 years-but real. If you have foot ulcers, poor circulation, or neuropathy, your doctor might avoid this drug.
Who Should and Shouldn’t Take Them
These drugs aren’t for everyone. Here’s who benefits most:
- Type 2 diabetes with heart disease (prior heart attack, angina, or blocked arteries)
- Type 2 diabetes with heart failure (even if you don’t feel symptoms)
- Type 2 diabetes with chronic kidney disease (eGFR ≥30)
- People who need weight loss and can’t tolerate GLP-1 agonists
- Those who get frequent low blood sugar on insulin or sulfonylureas
Here’s who should avoid them:
- People with type 1 diabetes (high risk of DKA)
- eGFR below 30 mL/min (kidneys can’t handle it)
- Those with recurrent genital yeast infections
- People with a history of lower limb amputations (especially if on canagliflozin)
- Anyone with severe volume depletion or on high-dose diuretics
And if you’re young, healthy, and just have type 2 diabetes with no heart or kidney issues? The benefit is much smaller. One study found you’d need to treat 52 people for five years to prevent one major heart event. Is the cost and risk worth it? Maybe not.
Cost, Access, and Real-World Hurdles
These drugs are expensive. A 30-day supply costs around $600 at retail. That’s why many patients stop taking them. A 2023 study found cost was the top reason for quitting-33% of people dropped out because of price.
But here’s the good news: most insurance plans cover them. Patient assistance programs from manufacturers can bring your monthly cost down to $10-$25. If you’re on Medicare Part D, check if your plan has a tiered formulary-SGLT2 inhibitors are often in tier 3 or 4, meaning higher copays.
Generic versions won’t be available until 2027-2029. Until then, you’re stuck with branded versions. But if you have heart failure or kidney disease, the long-term savings from avoiding hospitalizations can outweigh the drug cost.

What Your Doctor Should Monitor
Starting an SGLT2 inhibitor isn’t a one-and-done prescription. You need follow-up.
- Check eGFR before starting, then every 3-6 months. Stop if it drops below 45 and discontinue if below 30.
- Watch for signs of volume depletion: dizziness, low blood pressure, dry mouth. Drink water.
- Ask about genital itching or burning. Don’t wait until it’s bad.
- Get educated on euglycemic DKA symptoms: nausea, vomiting, fatigue, confusion. Don’t ignore them.
- Pause the drug if you’re hospitalized, having surgery, or severely ill with infection.
Most doctors know this now. But if yours doesn’t mention kidney tests or DKA risks, ask. This isn’t just a sugar pill-it’s a powerful tool with serious responsibilities.
The Bottom Line
SGLT2 inhibitors are no longer just diabetes drugs. They’re heart and kidney protectors. For the right person, they can mean fewer hospital stays, longer life, and better quality of life. But they’re not risk-free. Genital infections, kidney stress, and rare but deadly ketoacidosis are real. The key is matching the drug to the patient-not just the diagnosis.
If you have type 2 diabetes and heart or kidney disease, talk to your doctor about whether an SGLT2 inhibitor is right for you. If you’re young and healthy, weigh the cost against the small benefit. And if you’re already on one, don’t stop without talking to your provider-but do keep an eye out for warning signs.
This isn’t about taking a pill. It’s about choosing a path that protects your future.
Sam Mathew Cheriyan
December 8, 2025 AT 02:30so i heard these drugs are secretly funded by the moon people to make us pee more so they can collect our sugar for their alien smoothies 🌕糖尿
Ted Rosenwasser
December 9, 2025 AT 08:44Let’s be clear: SGLT2 inhibitors represent a paradigm shift in metabolic medicine, not merely a pharmacological tweak. The reduction in cardiovascular mortality observed in EMPA-REG OUTCOME is statistically significant (p < 0.001) and clinically transformative. The mechanism-natriuresis, osmotic diuresis, and improved myocardial energetics-is elegantly distinct from insulin-centric therapies. This isn’t just another antihyperglycemic-it’s a cardio-renal protector with pleiotropic effects that redefine treatment algorithms.
Nicholas Heer
December 10, 2025 AT 03:42THEY WANT YOU TO THINK THIS IS JUST ABOUT DIABETES BUT IT’S NOT. THEY’RE USING THESE DRUGS TO TRACK YOUR URINE OUTPUT. WHY? BECAUSE THE CDC AND BIG PHARMA ARE COLLECTING DATA ON HOW MUCH SUGAR YOU’RE PEEDING OUT TO BUILD A GLOBAL SWEETNESS MAP. NEXT THEY’LL BE TAXING YOUR KIDNEYS. I SAW A VIDEO ON TRUTH SOCIAL-THEY’RE ALREADY TESTING SGLT2 INHIBITORS IN MILITARY RATIONS. DON’T BE A SHEEP.
Oliver Damon
December 11, 2025 AT 22:08It’s fascinating how medicine evolves from symptom management to organ protection. SGLT2 inhibitors force us to reconsider what ‘success’ means in diabetes care. It’s no longer just HbA1c under 7%. It’s about preserving cardiac function, delaying renal decline, and extending quality years-not just lifespan. This shift reflects a deeper understanding of metabolic disease as a systemic disorder. We’re moving from glucose-centric to patient-centric outcomes. That’s not just science-it’s wisdom.
Ryan Sullivan
December 13, 2025 AT 03:57Let’s not pretend this is magic. These drugs cause yeast infections, dehydration, and rare but catastrophic ketoacidosis. The benefits are real, but the marketing is overhyped. If you’re a 45-year-old with prediabetes and no comorbidities, you’re paying $600/month to lose 3 kilos and pee more. That’s not a treatment-it’s a lifestyle accessory for the overmedicated.
Wesley Phillips
December 14, 2025 AT 18:27My doc put me on Jardiance after my heart scare and honestly? I feel like a new man. Lost 12 lbs in 2 months, BP down, no crashes. Yeah I got a yeast infection-used Monistat and moved on. This isn’t a sugar pill. It’s a life upgrade. 🚀
Desmond Khoo
December 16, 2025 AT 17:46if you’re on one of these and feel weirdly tired or nauseous-DON’T IGNORE IT. I thought i had the flu but it was euglycemic DKA. ended up in the er. they saved me but man. if you’re reading this and on SGLT2-keep water close and know the signs. you’re not alone 💙
David Brooks
December 18, 2025 AT 03:27THIS IS THE MOST IMPORTANT MEDICAL ADVANCE SINCE STATINS. I’M NOT EXAGGERATING. PEOPLE ARE LIVING LONGER, HAVING LESS HOSPITAL STAYS, AND KEEPING THEIR KIDNEYS BECAUSE OF THIS. IF YOUR DOCTOR ISN’T TALKING TO YOU ABOUT THIS-FIND A NEW ONE. THIS ISN’T A DRUG. IT’S A REVOLUTION.
Jennifer Anderson
December 19, 2025 AT 04:26i had kidney disease and was scared to start anything new. my nurse practitioner sat with me for 45 mins, explained the risks, and helped me apply for the patient program. now my eGFR is stable and i’m not on dialysis. these drugs saved my life. if you’re hesitant, ask for help. you don’t have to figure it out alone 🌱
Kurt Russell
December 20, 2025 AT 14:46you think you’re just taking a pill to lower sugar. you’re not. you’re signing up for a new lease on life. i went from needing a cane to hiking 5 miles last weekend. yes, i got a UTI. yes, i had to pause it before surgery. but the trade-off? worth every second. this isn’t medicine-it’s a second chance.
Kyle Oksten
December 22, 2025 AT 04:14There’s a reason these drugs are now first-line for patients with heart failure or CKD: the evidence is overwhelming. But we must also acknowledge the limitations. Not everyone benefits equally. Cost, access, and side effect profiles demand personalized decision-making. Medicine isn’t about one-size-fits-all-it’s about matching the right tool to the right person. SGLT2 inhibitors are powerful, but they’re not universal solutions.
Helen Maples
December 22, 2025 AT 13:59Stop romanticizing these drugs. The amputation risk with canagliflozin isn’t a footnote-it’s a red flag. I’ve seen patients lose toes because their doctor didn’t screen for peripheral neuropathy. This isn’t a ‘cool new pill.’ It’s a high-stakes intervention. If you’re not checking feet, eGFR, and volume status every 3 months-you’re not practicing medicine. You’re gambling.
Sadie Nastor
December 23, 2025 AT 21:48my mom’s on Farxiga and she says it’s the best thing that’s happened since her grandkid was born 😊 she lost weight, feels less tired, and even started gardening again. yeah she had a yeast thing but used yogurt and it went away. i’m so glad she didn’t give up. if you’re scared, start small. talk to your doc. you got this 💕