QT Prolongation: What It Is, Why It Matters, and Which Medications Can Cause It
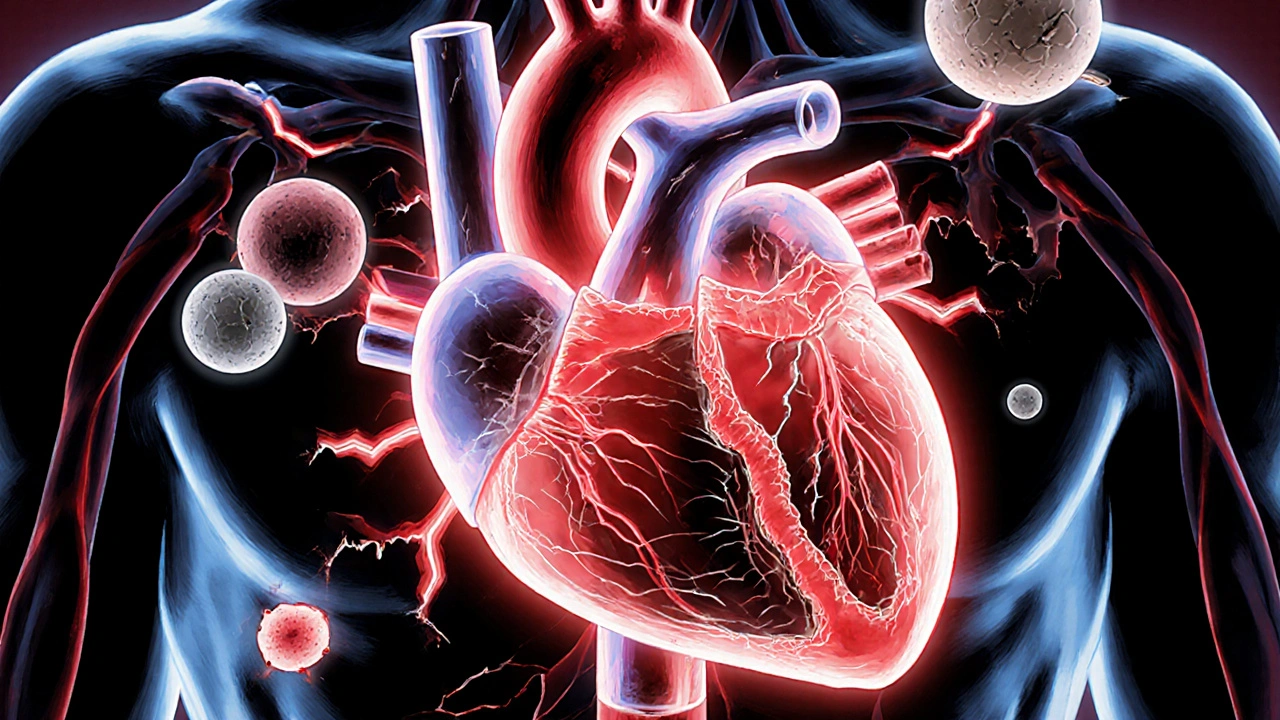
When your heart’s electrical system takes too long to reset between beats, it’s called QT prolongation, a delay in the heart’s repolarization phase that can trigger life-threatening irregular rhythms. Also known as long QT syndrome, it’s not always genetic—many cases are caused by medications you might be taking right now. This isn’t just a lab number. It’s a real risk that can turn a routine prescription into a silent danger.
Some drugs directly interfere with the ion channels that control your heart’s rhythm. Antibiotics, like erythromycin and moxifloxacin, can slow down the heart’s recovery phase. Antidepressants, including citalopram and escitalopram, are common culprits too. Even anti-nausea meds, such as ondansetron, have been linked to QT changes. These aren’t rare side effects—they’re documented, predictable, and often overlooked because they don’t show up until something serious happens.
It’s not just about the drug. Electrolyte imbalance, especially low potassium or magnesium, makes QT prolongation much more likely. If you’re on diuretics, have kidney issues, or eat poorly, your risk goes up—even if your meds are fine on paper. And it’s worse if you’re older, female, or already have heart disease. This isn’t theoretical. People have gone into cardiac arrest from a simple antibiotic combo they didn’t know could interact.
You won’t feel QT prolongation until it’s too late. No chest pain. No dizziness. Just a sudden, unpredictable rhythm called torsades de pointes, a type of ventricular tachycardia that can turn fatal in seconds. That’s why doctors check ECGs before starting certain drugs and why you should never mix multiple medications without knowing the risks.
What you’ll find in these posts isn’t just a list of dangerous drugs. It’s a practical guide to what actually matters: which medicines carry the highest risk, how to spot hidden triggers, and what steps to take if you’re already on something that could affect your heart. You’ll see real cases—like how turmeric supplements spiked INR levels in people on blood thinners, or why certain pain meds can be risky for people with existing heart conditions. These aren’t abstract warnings. They’re survival tips disguised as medication guides.
Heart Arrhythmias from Medications: Warning Signs and How to Manage Them
Over 400 common medications can trigger dangerous heart rhythm problems. Learn the warning signs - like palpitations, dizziness, and fainting - and how to manage drug-induced arrhythmias safely before they become life-threatening.
learn moreAntipsychotics and QT-Prolonging Drugs: What You Need to Know About Heart Risks
Combining antipsychotics with other QT-prolonging drugs can trigger dangerous heart rhythms. Learn which medications raise the risk, who's most vulnerable, and how to stay safe with simple monitoring steps.
learn more