QT Prolongation Risk Calculator
When you're taking an antipsychotic for schizophrenia, bipolar disorder, or severe depression, your doctor focuses on calming your mind. But there's another system in your body that’s quietly at risk: your heart. Mixing certain antipsychotics with other common medications can stretch out your heart’s electrical cycle-known as QT prolongation-and trigger a life-threatening rhythm called torsades de pointes. This isn’t theoretical. Between 2010 and 2022, the FDA documented 128 cases of this dangerous arrhythmia directly tied to drug combinations. And it’s happening more than you think.
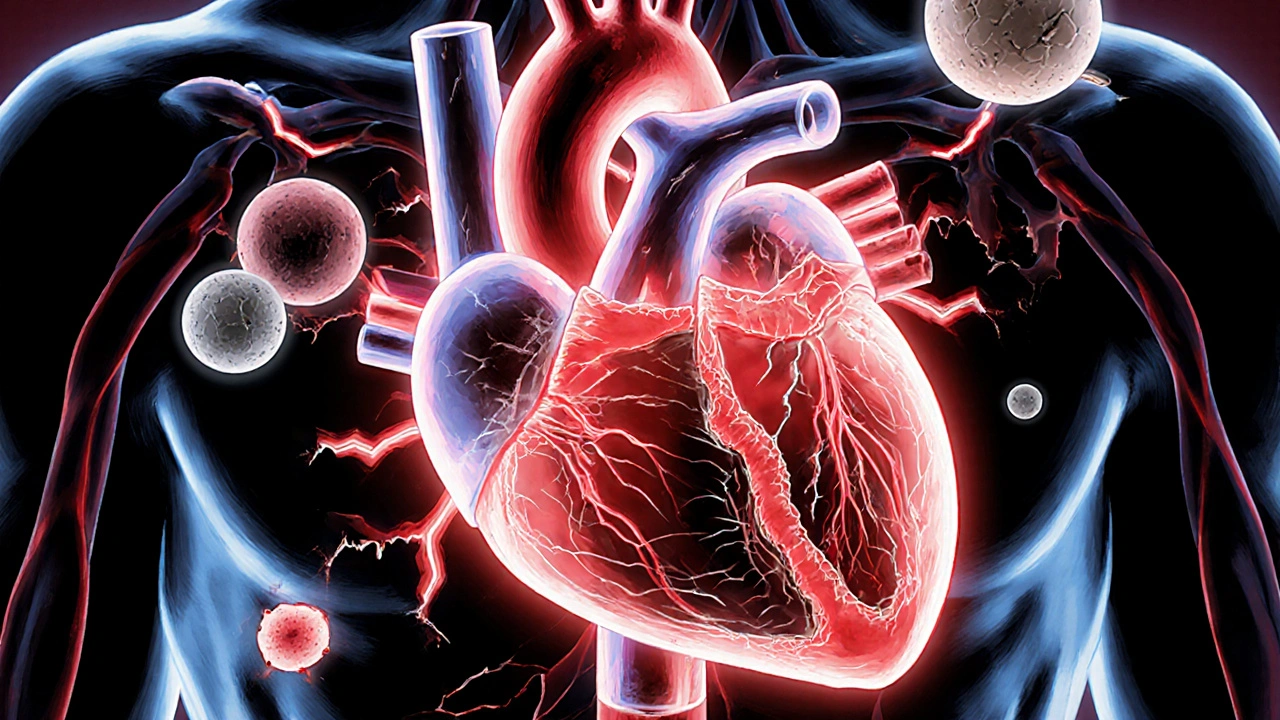
How QT Prolongation Works
Your heart beats because of electrical signals. After each beat, the heart muscle needs to reset-this is called repolarization. The QT interval on an ECG measures how long that reset takes. If it’s too long, the heart can misfire. Normal QTc (corrected QT) is under 440 ms for men and under 460 ms for women. When it hits 500 ms or more, your risk of sudden cardiac arrest jumps fivefold. The culprit? Many antipsychotics block the hERG potassium channel. This channel helps the heart recharge after beating. When it’s blocked, the reset takes longer. Some drugs are worse than others. Thioridazine, for example, has an IC50 of just 0.04 μM-meaning it blocks hERG at very low doses. Ziprasidone and haloperidol are also high-risk. Even common ones like quetiapine and risperidone can do it, especially when stacked with other meds.Which Drugs Make the Risk Worse?
It’s not just antipsychotics. Many everyday drugs also prolong QT. Antibiotics like moxifloxacin and ciprofloxacin. Anti-nausea drugs like ondansetron. Even some antidepressants and heart medications like sotalol. When you combine them, the effect isn’t just added-it’s multiplied. A 2021 study from the University of Pennsylvania found that combining an antipsychotic with another QT-prolonging drug led to 2.3 to 4.7 times more QT prolongation than either drug alone. One case from Cleveland Clinic showed a 68-year-old woman’s QTc jumping from 448 ms to 582 ms in just three days after starting quetiapine and ciprofloxacin together. She nearly died. Here’s how common this is: 45% of people on antipsychotics are also taking at least one other drug that affects QT. That’s nearly half of all patients. And most don’t know it.Who’s at Highest Risk?
Some people are more vulnerable. Age matters. If you’re over 65, your QT interval naturally runs longer-by about 15.3 ms. Women are at higher risk too, with an average 12.8 ms longer QTc than men. Low potassium (below 3.5 mmol/L) adds another 22.7 ms. Slow heart rate (under 50 bpm) adds 18.4 ms. All of these stack up. That’s why a 70-year-old woman with low potassium, taking risperidone and ondansetron, is in a danger zone. Her QTc might creep past 500 ms without any warning signs. She might feel fine-no chest pain, no dizziness-until her heart skips into torsades de pointes. And that’s often fatal if not caught fast.
Which Antipsychotics Are Safer?
Not all antipsychotics carry the same risk. Aripiprazole, brexpiprazole, and lurasidone have very weak hERG blockade. Their IC50 values are over 10 μM-meaning they barely touch the potassium channel. Studies show aripiprazole has almost no increased risk of sudden death compared to not taking any antipsychotic. Brexpiprazole’s risk is even slightly lower. Despite this, high-risk drugs like quetiapine and risperidone are still prescribed far more often. In 2023, quetiapine had over 24 million prescriptions in the U.S. Why? It’s cheap, effective for sleep and agitation, and many doctors aren’t trained to think about heart risks. But the tide is turning. Low-risk antipsychotics now make up 38% of new prescriptions-up from 22% in 2019. By 2027, that number could hit 52%, thanks to Medicare’s new quality rules.What Should You Do?
If you’re on an antipsychotic, ask these questions:- Is my drug on the high-risk list?
- Am I taking any antibiotics, anti-nausea meds, or heart drugs?
- Have I had an ECG since starting this medication?
- Are my potassium and magnesium levels checked regularly?

How to Reduce the Risk
You don’t have to live in fear. There are proven ways to stay safe.- Check electrolytes. Potassium and magnesium are the first line of defense. A 2023 JAMA Cardiology study found that regular monitoring prevented 82% of torsades cases in high-risk patients.
- Use low-risk antipsychotics when possible. If your symptoms are stable, ask your doctor if switching to aripiprazole or lurasidone is an option.
- Avoid combo triggers. Don’t take ondansetron if you’re on ziprasidone. Don’t take ciprofloxacin if you’re on haloperidol. Ask your pharmacist to run a drug interaction check every time a new med is added.
- Consider a digital ECG patch. The FDA approved the Zio XT patch in May 2024 for psychiatric patients. It’s worn for up to 14 days and catches QT spikes you’d miss with a single ECG. It’s 98.7% accurate at detecting dangerous prolongation.
The Bigger Picture
This isn’t just about individual patients. The U.S. spends $1.2 billion a year on unnecessary ECGs for low-risk people, while high-risk patients go unmonitored. Meanwhile, Medicare is now tying 2.3% of Part D payments to whether doctors follow QT monitoring guidelines. That’s a big change. The European Medicines Agency now requires antipsychotic labels to include clear tables showing which drug combinations are dangerous. The American Psychiatric Association is rolling out a risk calculator in early 2025 that factors in age, sex, electrolytes, and all meds you’re taking. And by 2026, a genetic test will identify people who metabolize antipsychotics slowly-making them 2.4 times more likely to overdose on standard doses. The goal? Reduce torsades to fewer than 1 case per 100,000 patient-years. That’s achievable-if we stop ignoring the heart while treating the mind.Can antipsychotics cause sudden death?
Yes, but it’s rare and usually preventable. Sudden death from antipsychotics is most often due to torsades de pointes, a dangerous heart rhythm triggered by QT prolongation. This happens mostly when antipsychotics are combined with other QT-prolonging drugs like antibiotics or anti-nausea meds. The absolute risk is low-about 1 in 25,000 patient-years-but it’s preventable with proper monitoring.
Which antipsychotic is safest for the heart?
Aripiprazole, brexpiprazole, and lurasidone are the safest options. They have very weak effects on the hERG potassium channel, which means they rarely cause QT prolongation. Studies show aripiprazole carries no statistically significant increase in sudden cardiac death risk compared to not taking any antipsychotic. These are now preferred for patients with heart conditions or those on multiple medications.
Do I need an ECG if I’m on an antipsychotic?
Yes-if you’re on a high- or moderate-risk antipsychotic like haloperidol, ziprasidone, risperidone, or quetiapine. Guidelines recommend a baseline ECG within one week of starting the drug. If you’re also taking another QT-prolonging medication, you need weekly ECGs for the first month, then monthly. Even if you feel fine, silent QT prolongation can happen without symptoms.
Can I take antibiotics while on an antipsychotic?
Some antibiotics are safe, others are dangerous. Fluoroquinolones like ciprofloxacin and moxifloxacin strongly prolong QT and should be avoided with high-risk antipsychotics. Azithromycin and amoxicillin are generally safe. Always check with your pharmacist before starting any new antibiotic. Never assume it’s okay just because it’s common.
Why aren’t doctors always checking QT intervals?
Many reasons. Insurance often denies repeat ECGs. Rural clinics don’t have ECG machines. Some doctors don’t know the guidelines. Others think the risk is too low to worry about. But studies show that when clinics use electronic alerts and follow protocols, dangerous drug combinations drop by over 50%. It’s not about overtesting-it’s about smart, targeted monitoring.
What should I do if I’m scared to take my antipsychotic?
Don’t stop on your own. Talk to your doctor about switching to a low-risk antipsychotic like aripiprazole. Ask for a baseline ECG and blood tests for potassium and magnesium. Many patients feel better once they understand the real risk-it’s low if you’re monitored. Fear of heart problems caused 29% of patients to quit their meds, but most of those cases could have been avoided with simple safety steps.
Elizabeth Nikole
October 31, 2025 AT 16:25LeAnn Raschke
November 2, 2025 AT 01:49Adorable William
November 2, 2025 AT 09:50Suresh Patil
November 4, 2025 AT 08:45Ram Babu S
November 4, 2025 AT 20:42Kyle Buck
November 6, 2025 AT 10:43Amy Craine
November 7, 2025 AT 11:25Alicia Buchter
November 9, 2025 AT 07:07MaKayla VanMeter
November 10, 2025 AT 20:56Doug Pikul
November 11, 2025 AT 01:38anthony perry
November 11, 2025 AT 03:16Sarah Major
November 11, 2025 AT 08:33Craig Venn
November 11, 2025 AT 10:12Amber Walker
November 12, 2025 AT 20:29