Opioid Withdrawal Management: What Works and What to Avoid
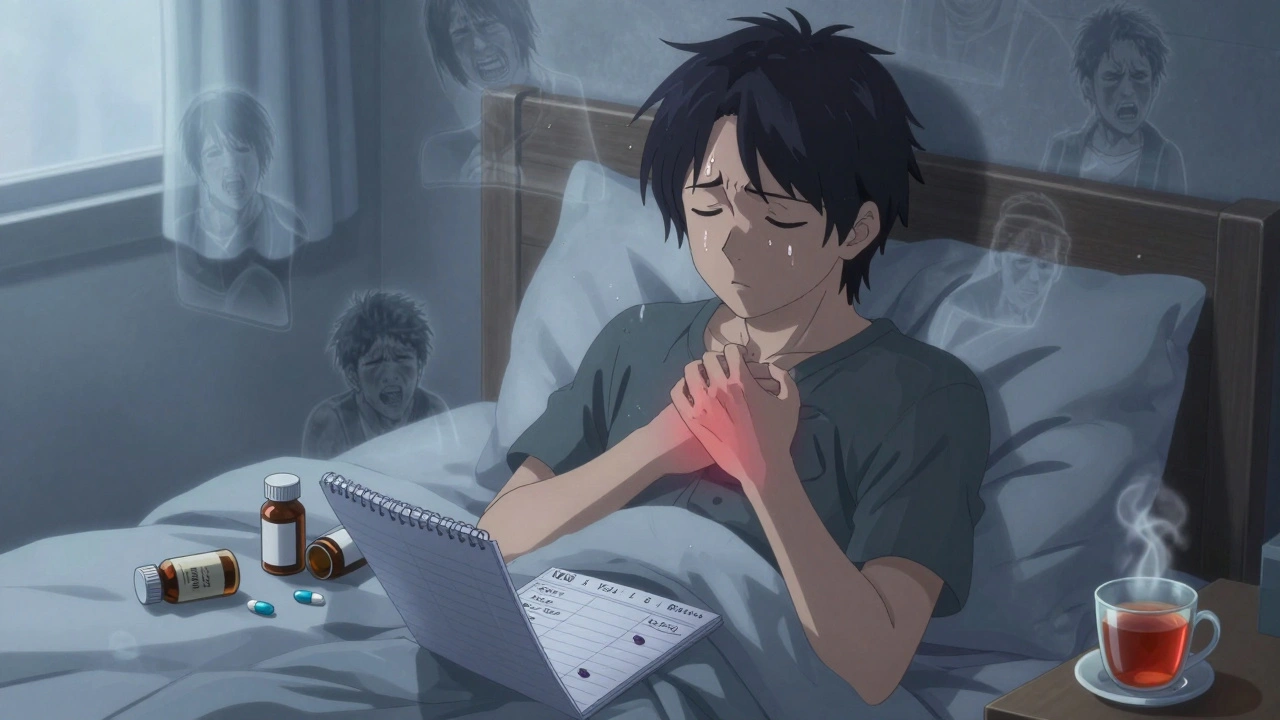
When someone stops using opioids after regular use, their body goes through opioid withdrawal management, the process of safely reducing dependence and managing physical and emotional symptoms that follow cessation. Also known as opioid detox, it’s not just about gritting your teeth—it’s a medical process that needs structure, support, and sometimes medication to avoid relapse or worse. Many people think withdrawal is just flu-like symptoms—sweating, nausea, muscle aches—but it’s more than that. It’s a neurological reset. Your brain has adapted to opioids being present, and when they’re gone, it scrambles to regain balance. That’s why cold turkey often fails, and why professional guidance matters.
Medication-assisted treatment, the use of FDA-approved drugs like methadone, buprenorphine, or naltrexone to ease withdrawal and reduce cravings is the gold standard for most cases. It’s not swapping one drug for another—it’s stabilizing your system so you can focus on recovery. Studies show people using these medications are far more likely to stay in treatment and avoid overdose. Then there’s naloxone, a life-saving drug that reverses opioid overdose by blocking opioid receptors in the brain. While naloxone doesn’t treat withdrawal, it’s a critical safety net for anyone in early recovery, especially since tolerance drops quickly after stopping use, making overdose more likely if they relapse.
What doesn’t work? Going it alone without support. Home remedies like hot baths, herbal teas, or over-the-counter painkillers might ease a few symptoms, but they won’t stop the intense cravings or anxiety that drive relapse. And don’t trust online myths—some people claim fasting or extreme exercise helps, but those can actually worsen dehydration or heart strain during withdrawal. Real progress comes from knowing your limits and having a plan. Whether you’re asking for help for yourself or someone else, the goal isn’t just to get through the worst days—it’s to build a future where opioids aren’t needed to feel okay.
The posts below cover real-world experiences and science-backed strategies—from how to track withdrawal symptoms safely, to understanding how medications like buprenorphine work in the body, to what to do when someone you care about is struggling. You’ll find practical advice on avoiding triggers, managing sleep and mood swings, and knowing when to seek emergency help. No fluff. No judgment. Just what you need to move forward.
Opioid Withdrawal: How to Safely Taper and Manage Symptoms
Learn how to safely taper off opioids with a step-by-step guide to managing withdrawal symptoms, using medications, and building long-term recovery. Based on CDC guidelines and real patient outcomes.
learn more