Opioid Detox: What It Really Takes to Safely Quit
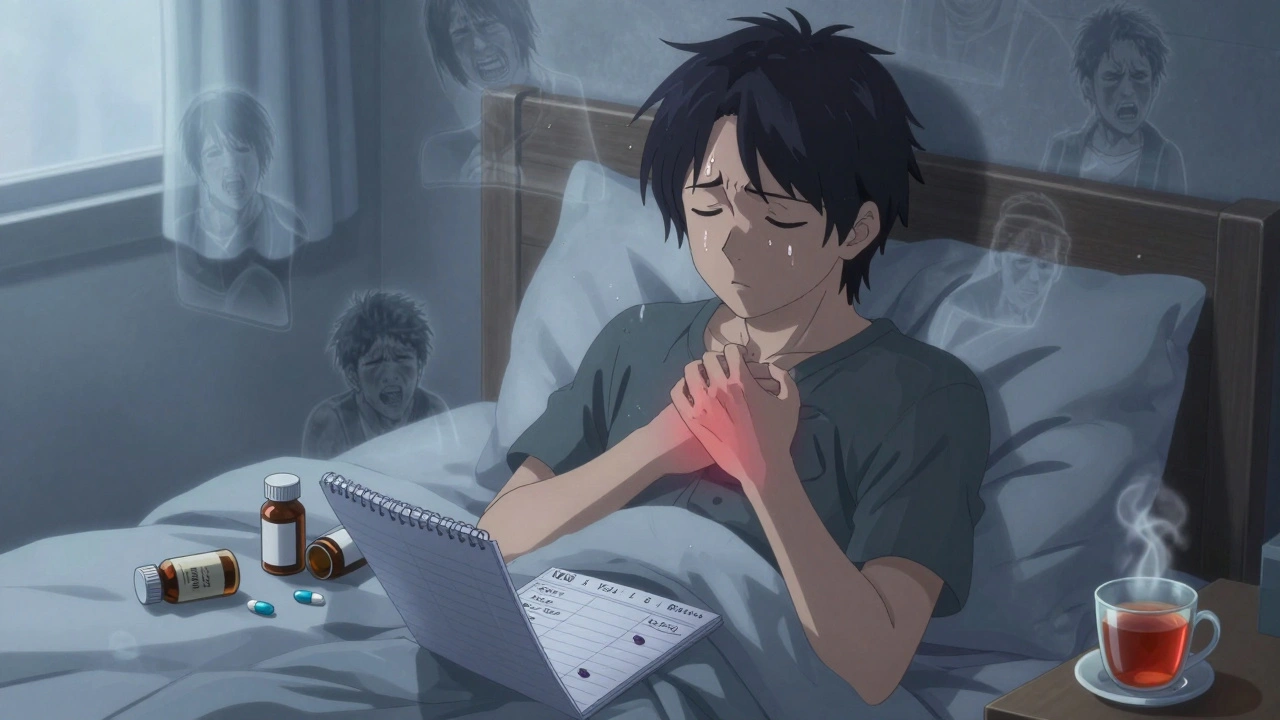
When someone stops using opioids like heroin, fentanyl, or prescription painkillers, their body goes through opioid detox, the process of clearing opioids from the system while managing withdrawal symptoms. Also known as withdrawal management, it’s not a cure—but it’s the essential first step before real recovery can begin. This isn’t like quitting caffeine or sugar. Opioids change how your brain works, and when you stop, your nervous system goes into overdrive. You don’t just feel bad—you might sweat, shake, vomit, have muscle cramps, and feel like you can’t breathe. It’s intense. And it’s dangerous if you try to do it alone.
Opioid withdrawal, the physical and emotional reaction when opioids leave your system usually starts within hours after the last dose and peaks around day 2 or 3. For some, symptoms last a week. For others, cravings and anxiety drag on for months. That’s why medical support matters. You can’t just tough it out. Clinics use medications like methadone or buprenorphine to ease symptoms, and sometimes clonidine to calm the nervous system. But the most critical tool? naloxone, a life-saving drug that reverses opioid overdose. Even if you’re detoxing to get clean, someone nearby should have naloxone on hand. Overdose risk is highest right after detox because your tolerance drops. A dose that used to feel normal can kill you now.
Detox isn’t the end—it’s the beginning. And it’s not just about the body. The emotional side is just as heavy. Shame, fear, isolation. Many people relapse because they don’t have real support after detox ends. That’s why programs that combine medical care with counseling, peer groups, and job help work better. You need more than a pill. You need a plan. And you need people who’ve been there.
What you’ll find below are real, practical guides on what happens during detox, how to recognize an overdose, why naloxone is non-negotiable, and how to avoid common mistakes that send people back to opioids. These aren’t theory pieces. They’re written by people who’ve seen this up close—from emergency rooms to recovery centers. If you’re detoxing, helping someone who is, or just trying to understand what’s really going on—this collection gives you what you need to stay safe and make smarter choices.
Opioid Withdrawal: How to Safely Taper and Manage Symptoms
Learn how to safely taper off opioids with a step-by-step guide to managing withdrawal symptoms, using medications, and building long-term recovery. Based on CDC guidelines and real patient outcomes.
learn more