Clostridioides difficile: Causes, Risks, and What You Need to Know
When you take antibiotics, you’re not just killing bad bacteria—you’re also wiping out the good ones that keep your gut in balance. That’s when Clostridioides difficile, a hardy, spore-forming bacterium that thrives when gut flora is disrupted. Also known as C. diff, it can take over and cause severe diarrhea, fever, and even life-threatening colon inflammation. It’s not just a hospital problem—it’s now showing up in people who’ve never set foot in a medical facility.
C. diff spreads through spores that survive on surfaces for months. If you touch a doorknob, toilet handle, or bed rail contaminated with fecal matter from an infected person, and then touch your mouth, you could get infected. This is why handwashing with soap and water (not just hand sanitizer) is critical—alcohol-based gels don’t kill the spores. People over 65, those on long-term antibiotics, and anyone with a weakened immune system are at highest risk. But even healthy adults can catch it after a simple course of amoxicillin or clindamycin.
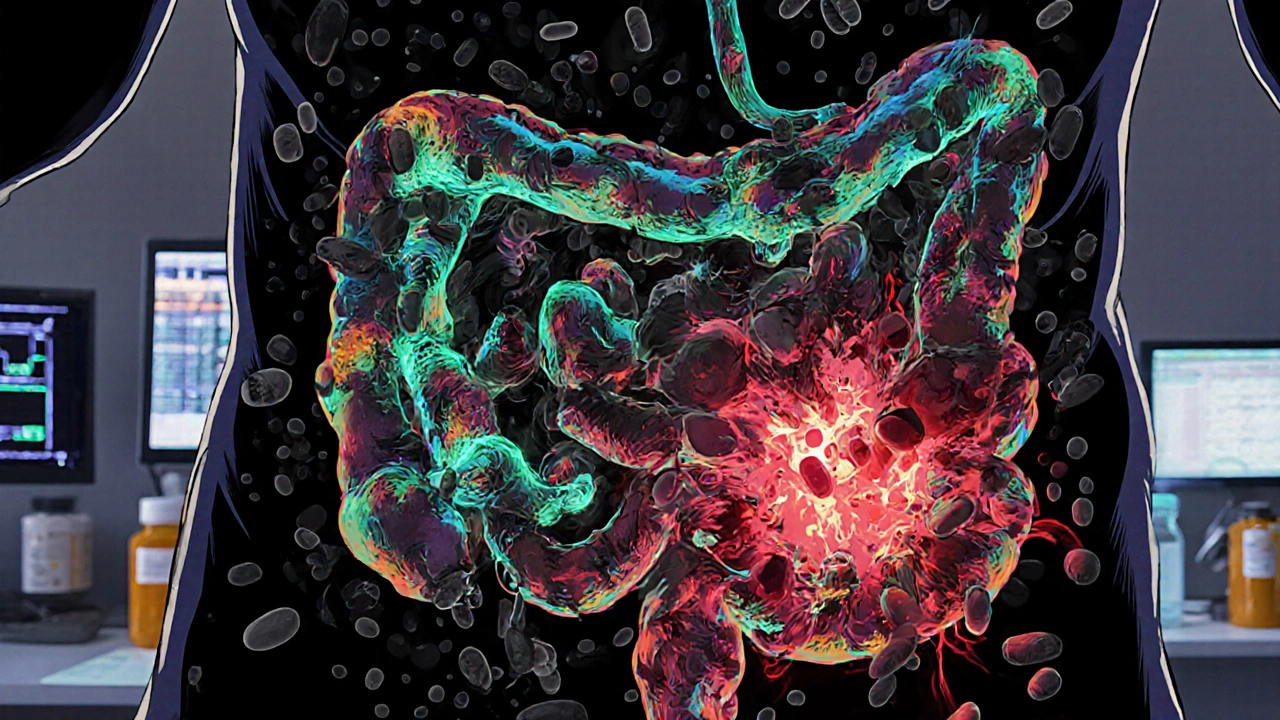
The real danger? Once C. diff takes hold, it releases toxins that destroy the lining of your colon. Symptoms start with watery diarrhea, then can escalate to blood or pus in stool, intense abdominal pain, and dehydration. Recurrence is common—about 1 in 5 people get it again after treatment. And when standard antibiotics like vancomycin fail, fecal microbiota transplants (FMT) are now being used to restore healthy gut bacteria. This isn’t science fiction—it’s a proven, FDA-approved therapy for stubborn cases.
What you won’t find in most patient guides is how often C. diff is misdiagnosed. Doctors sometimes mistake it for food poisoning or viral gastroenteritis. If you’ve been on antibiotics recently and develop diarrhea that lasts more than two days, ask for a stool test. Early detection saves lives. And if you’re caring for someone with C. diff, know that cleaning with bleach-based products is non-negotiable. Regular disinfectants won’t cut it.
The posts below dive into how drug interactions, antibiotic use, and hospital protocols connect to C. diff outbreaks. You’ll find real-world insights on managing infections, avoiding recurrence, and understanding why some meds make you more vulnerable—not just what to take, but what to avoid. Whether you’re a patient, caregiver, or just someone trying to stay healthy after antibiotics, this collection gives you the facts you need to protect yourself.
Clostridioides difficile: Understanding Antibiotic-Associated Diarrhea and How to Prevent It
Clostridioides difficile (C. diff) is the leading cause of antibiotic-associated diarrhea, causing severe colitis and recurring infections. Learn how antibiotics trigger it, how it's diagnosed and treated today, and the proven ways to prevent it.
learn more