Most prescriptions you get filled are generics. In fact, 90% of all prescriptions in the U.S. are for generic drugs. They work just as well, cost a fraction of the price, and are approved by the FDA. So why would your doctor ever write a prescription that says "do not substitute" or "brand medically necessary"? It’s not because they’re ignoring cost or pushing you to spend more. Sometimes, it’s because the difference between a brand and a generic isn’t just about price-it’s about safety.
When the Difference Actually Matters
Not all drugs are created equal when it comes to switching between brand and generic. For some medications, even tiny changes in how your body absorbs the drug can lead to serious problems. These are called narrow therapeutic index (NTI) drugs. With NTI drugs, the line between a therapeutic dose and a toxic one is thin. A 5% change in blood levels might mean your seizure returns, your blood clots, or your thyroid stops working right. That’s why doctors often stick with brand names for drugs like:- Levothyroxine (Synthroid, Tirosint): Used for hypothyroidism. Even small changes in hormone levels can cause fatigue, weight gain, or heart rhythm issues. The American Thyroid Association recommends staying on the same brand because generics vary in inactive ingredients that affect absorption.
- Levetiracetam (Keppra): An anti-seizure medication. A 2019 study found that 12.7% of patients switched to generic versions had breakthrough seizures, compared to just 4.3% who stayed on brand.
- Warfarin (Coumadin): A blood thinner. A 2% difference in concentration can mean a stroke or a dangerous bleed. Many doctors avoid switching patients on warfarin unless absolutely necessary.
For these drugs, the FDA’s standard-generic drugs must be within 80-125% of the brand’s absorption rate-isn’t enough. That 45% window is too wide when your life depends on precision.
Why Doctors Still Use Brand Names (Even When They Don’t Need To)
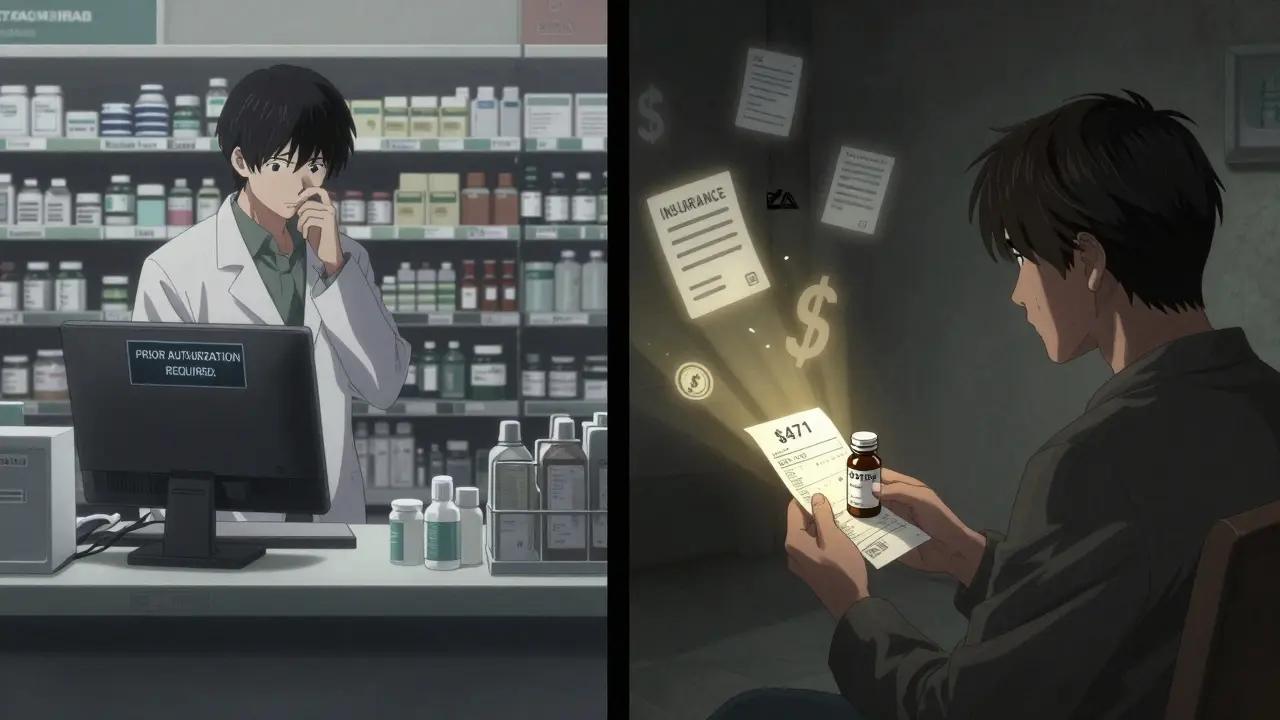
Here’s the uncomfortable truth: a lot of the time, doctors prescribe brand-name drugs not because of science-but because of habit. A 2018 study of over a million doctor’s notes found that physicians use brand names in 15-20% of cases, even when generics are available and approved. Why? Because they’re trained on brand names. They see them on TV ads. Their reps show up with samples. They remember the name from med school. It’s not always intentional. One study showed that when doctors write "Keppra," patients are more likely to ask for Keppra-even if the generic is identical. And pharmacists, under state law, can’t switch it unless the doctor says "substitute." This isn’t just about confusion. It’s about money. Brand-name drugs cost 80-85% more than generics. A 2022 GoodRx report showed the average brand-name prescription cost $471.67. The generic? $13.76. When a doctor writes a brand-only prescription without a clear medical reason, it can cost patients hundreds-or even thousands-of dollars a year. Insurance might cover it, but often only after a long prior authorization process. Or worse, you’re stuck paying out of pocket.What’s Really in the Pill? Inactive Ingredients Matter More Than You Think
You might think a generic is just the same active ingredient in a cheaper bottle. But the pill isn’t just the drug. It’s also the fillers, dyes, binders, and coatings. These are called inactive ingredients. And for some people, they make a huge difference. Take ciprofloxacin, a common antibiotic. Generic versions from different manufacturers use different fillers. Some patients report stomach upset, nausea, or diarrhea with one generic but not another. One Reddit user wrote: "I switched from brand to generic cipro and spent three days in bed. Switched back-back to normal in 24 hours." Same thing happens with levothyroxine. Patients report mood swings, hair loss, and weight changes after switching to a different generic brand. That’s not the thyroid hormone changing-it’s the lactose, cornstarch, or coloring agents affecting how the drug is absorbed in the gut. The FDA doesn’t require generics to match the brand’s inactive ingredients. So if you’ve had a bad reaction to one generic, it doesn’t mean all generics are bad. It just means you need to stick with the one that works for you. That’s when a doctor writes "do not substitute"-not because the drug is different, but because you are different.
Insurance, Prior Authorization, and the Bureaucratic Hurdle
If your doctor writes "brand medically necessary," your insurance doesn’t just approve it automatically. They’ll likely require a prior authorization. That means your doctor has to fill out paperwork explaining why the generic won’t work. The insurance company reviews it. This can take 24-72 hours. Approval rates vary. For antiepileptics like Keppra, insurers approve brand-only requests 89% of the time. For proton pump inhibitors (like omeprazole), it’s only 45%. Why? Because the evidence for needing the brand is strong for seizures, weak for heartburn. If your doctor doesn’t explain it clearly, your prescription might get denied. You’ll end up at the pharmacy, paying $400 for a drug you could’ve gotten for $15. And if you don’t pick it up? Your condition might worsen. Some states make this harder. California requires doctors to check a "Medical Necessity" box on electronic prescriptions. New York demands a written clinical reason. Other states? Just say "do not substitute" and you’re done.What You Can Do: Ask the Right Questions
You don’t have to accept a brand-only prescription without understanding why. Here’s what to ask:- "Is there a generic version?" If yes, ask: "Is this one of those drugs where the generic might not work the same?"
- "What happens if I try the generic?" For most drugs, nothing. For NTIs, your doctor should explain the risk.
- "Have other patients had problems switching?" This opens the door to real-world experience, not just textbook answers.
- "Can we try the generic and monitor how I feel?" Many doctors will agree, especially if you’re stable and have no history of bad reactions.
Also, check your pharmacy’s substitution policy. Some pharmacies will call your doctor before switching-even if the law allows it. That’s a good sign. It means they care about your safety, not just cost.
When Generic Is Perfectly Fine (And Often Better)
For most medications, generics are not just cheaper-they’re just as good. A 2020 JAMA meta-analysis of 47 studies with over 112,000 patients found no difference in outcomes between brand and generic versions of:- Statins (atorvastatin, simvastatin)
- ACE inhibitors (lisinopril, enalapril)
- SSRIs (sertraline, fluoxetine)
- Metformin for diabetes
One patient summed it up on a Consumer Reports survey: "I saved $1,200 a year switching my statin to generic. My cholesterol is the same. I feel the same. Why pay more?"
For these drugs, the brand offers no benefit. Only cost. And that cost gets passed on-in higher premiums, higher copays, higher prices for everyone.
The Bigger Picture: Why This Isn’t Just About You
Every time a doctor writes a brand-only prescription without a medical reason, it’s not just your wallet that’s affected. It’s the whole system. U.S. drug spending is over $1.3 trillion a year. Generics make up 90% of prescriptions but only 23% of that cost. If just 10% of unnecessary brand prescriptions were switched to generics, the U.S. could save $10 billion a year. That money could fund better care for chronic conditions, lower insurance premiums, or reduce out-of-pocket burdens for seniors on fixed incomes. The pharmaceutical industry argues that brand-name profits fund future innovation. But the truth? Most new drugs are extensions of old ones-slightly reformulated versions that extend patents, not breakthroughs. The real innovation comes from public research, academic labs, and government-funded science.What’s Changing? And What’s Not
The FDA is starting to pay attention. In 2023, they released new guidance asking generic manufacturers to match brand drugs in shape, size, and color. Why? To reduce confusion. Patients often think a different-looking pill is a different drug-and stop taking it. "Authorized generics" are also growing. These are made by the brand company but sold under a generic label. They’re identical to the brand, just cheaper. No variation in fillers. No risk of switching. And they’re becoming more common for high-risk drugs. Still, the problem persists. Drug reps still visit doctors. Marketing still pushes brand names. Patients still ask for them. And without clear education, doctors keep prescribing them out of habit.Bottom Line: Trust the Science, Not the Label
Most of the time, generic drugs are safe, effective, and cheaper. No downsides. But for a small group of drugs-those with narrow therapeutic windows, or when you’ve had a bad reaction before-brand names matter. Not because they’re better. But because your body is sensitive. And that’s worth protecting. Ask questions. Know your meds. If your doctor prescribes a brand-only, ask why. If they say "because it’s better," ask for proof. If they say "it’s what I always use," ask if they’ve checked the latest guidelines. Your health isn’t about the name on the bottle. It’s about what works for you.Can a pharmacist substitute a generic if the doctor says "do not substitute"?
No. In 49 states and Washington D.C., pharmacists are required to follow the prescriber’s instructions. If the prescription says "do not substitute," "dispense as written," or "brand medically necessary," the pharmacist cannot switch to a generic-even if it’s FDA-approved. Only Texas has different rules for certain drug classes, but even there, the doctor’s directive overrides substitution.
Why do some generics make me feel worse than the brand?
The active ingredient is the same, but the fillers, dyes, and coatings can differ between generic manufacturers. For some people, these inactive ingredients cause stomach upset, allergic reactions, or affect how the drug is absorbed. This is especially common with thyroid meds, antibiotics, and seizure drugs. If you notice a change after switching, tell your doctor and pharmacist. You may need to stick with the same brand or generic version that works for you.
Are brand-name drugs more effective than generics?
For the vast majority of medications-like blood pressure pills, cholesterol drugs, and antidepressants-no. Multiple large studies, including a 2020 JAMA meta-analysis of over 112,000 patients, show no difference in effectiveness or safety between brand and generic versions. The FDA requires generics to meet the same standards for strength, purity, and performance. The only exceptions are narrow therapeutic index drugs, where even small differences in absorption can matter.
What should I do if my insurance denies my brand-name prescription?
If your insurance denies coverage for a brand-name drug, your doctor can file a prior authorization appeal. They’ll need to explain why the generic won’t work for you-using clinical reasons, not just preference. If that fails, ask if an "authorized generic" (made by the brand company) is available. It’s often cheaper than the brand and identical in formulation. You can also check GoodRx or RxSaver for cash prices-sometimes the brand is cheaper out-of-pocket than the generic with insurance.
How can I tell if my medication is a narrow therapeutic index drug?
The FDA’s Orange Book lists therapeutic equivalence ratings. Drugs marked "AB1" or "AB2" are considered interchangeable. NTI drugs are often marked "TE" or "N" for non-interchangeable. Common ones include levothyroxine, warfarin, phenytoin, and cyclosporine. If you’re unsure, ask your pharmacist or doctor. You can also look up your drug on the FDA’s website or use a trusted app like Medscape or Epocrates.

Jillian Angus
December 23, 2025 AT 14:05My thyroid doctor made me switch generics once. I felt like a zombie for two weeks. Back to Synthroid and I’m fine. Not all generics are equal, even if the FDA says they are.
CHETAN MANDLECHA
December 24, 2025 AT 16:15Used to think generics were just rip-offs. Then I switched my blood pressure med to generic and saved $300/month. My BP didn’t budge. Why pay more if it’s the same?
Ajay Sangani
December 25, 2025 AT 07:14the fda is just another corp puppet. they let generics in because pharma owns them. i’ve seen people get sick from generics. it’s not coincidence. they want you dependent on their overpriced pills. check the patent dates. same company. same factory. different label.
Pankaj Chaudhary IPS
December 26, 2025 AT 10:50As a doctor in India, I see this daily. Patients come in asking for 'the American brand' because they think it's better. I explain generics are identical for 90% of drugs. But for warfarin or levothyroxine? We stick to one brand. Education is the key. Not marketing.
Gray Dedoiko
December 27, 2025 AT 17:14I had a bad reaction to a generic antibiotic. Felt like I was dying for 3 days. Switched back to the brand-felt normal in 12 hours. My pharmacist didn’t even ask. Just swapped it. Scary stuff.
Johnnie R. Bailey
December 27, 2025 AT 21:53It’s not about the pill. It’s about the person. My aunt has been on levothyroxine for 20 years. She’s tried three generics. Each one made her tremble, sleep 18 hours, and cry for no reason. Back to Synthroid? She’s human again. The FDA measures absorption. They don’t measure how a person feels. And that’s the whole point.
Generics are fine for statins. For thyroid? No. It’s not about cost. It’s about identity. Your body remembers what works. Don’t let a spreadsheet decide your quality of life.
The system is broken because it treats medicine like cereal. Buy the cheaper box. But your body isn’t a grocery shelf. It’s a symphony. One wrong note and everything falls apart.
And yes, doctors prescribe brand names out of habit. But sometimes, that habit is the only thing keeping someone alive.
Ask questions. Track your symptoms. If you feel off after a switch? Don’t shrug it off. Demand the original. Your life isn’t a cost-cutting exercise.
Also-authorized generics? That’s the real win. Same pill, same fillers, half the price. Why isn’t everyone pushing that?
suhani mathur
December 29, 2025 AT 02:30Oh wow, so now we’re blaming doctors for prescribing brand names? Let me guess-the real villain is Big Pharma paying them to do it. Right? Except I’ve been in clinics. Most docs don’t even know the price difference. They just know Keppra works. And if you’re having seizures, you don’t gamble with a new generic you’ve never seen before.
Also, the 12.7% seizure rate spike? That’s not anecdotal. That’s peer-reviewed. If you’re a parent of a kid with epilepsy, you don’t care about $15 vs $470. You care if your child dies.
And yes, generics are great for statins. But let’s not pretend this is a one-size-fits-all issue. It’s not. It’s nuanced. And that’s why we need doctors, not algorithms.
Chris Buchanan
December 29, 2025 AT 11:27So let me get this straight-your doctor writes 'do not substitute' because they're lazy, but you're mad when the pharmacy switches your seizure med and you have a fit? That’s not hypocrisy, that’s just capitalism.
Also, why do we still have brand reps in hospitals? It’s 2025. We have apps. We have databases. Yet somehow, a guy in a suit with free pens still influences prescriptions. We’re all just pawns in a $1.3 trillion game of Monopoly.
And yet, you’re surprised when someone gets sick from a different filler? Honey, your body isn’t a robot. It’s a messy, emotional, gluten-sensitive, lactose-intolerant, dye-averse biological miracle. Stop treating it like a spreadsheet.
Rosemary O'Shea
December 30, 2025 AT 14:34How quaint. You think the FDA is some benevolent guardian of health? Darling, they’re a regulatory shell game. The same company that makes Synthroid also makes the 'authorized generic.' Same factory. Same chemist. Same quality control. Just a different label. And you call that transparency? It’s theatrical capitalism at its finest.
And let’s not pretend that 'inactive ingredients' are harmless. They’re not. They’re the silent saboteurs of modern pharmacology. I once knew a woman who had a full-body rash from a generic omeprazole because of a dye. The label said 'inactive.' It was anything but.
It’s not about the drug. It’s about the narrative. We’ve been trained to believe cheaper = worse. And the pharmaceutical industry? They’ve monetized that fear.
So yes-ask questions. But don’t stop there. Demand reform. Demand transparency. Demand that the FDA stop pretending this is a science and admit it’s a market.
Ademola Madehin
December 31, 2025 AT 03:59Bro I switched my antidepressant to generic and I cried for 3 days straight. My wife thought I was cheating. I was just… gone. Back to brand? I’m human again. This isn’t about money. It’s about your soul being in a pill.
Jamison Kissh
January 1, 2026 AT 08:25It’s fascinating how we treat medicine like a commodity. We optimize for cost, efficiency, scalability. But the human body isn’t a factory line. It’s a unique ecosystem. One person’s inert filler is another person’s trigger. The FDA’s 80-125% window is mathematically sound. But biology doesn’t care about math.
Maybe we need a new classification-not just 'interchangeable' or 'not.' But 'personalized equivalence.' A system that tracks which generic version worked for you, and locks it in. Like a genetic passport for meds.
Until then? Trust your body. Track your symptoms. And if your doctor says 'it’s the same'-ask them to try it themselves for a month.
EMMANUEL EMEKAOGBOR
January 1, 2026 AT 20:47As someone from Nigeria where generics are the only option, I’ve seen both sides. Some generics save lives. Others cause harm. The difference isn’t always the drug-it’s the storage, the humidity, the supply chain. A pill that works in Ohio might rot in Lagos.
So when I see Americans arguing about Synthroid vs generic, I’m reminded: we’re not talking about the same system. For many, the question isn’t 'brand or generic'-it’s 'will I get any pill at all?'
Let’s not romanticize the American system. It’s broken. But it’s still better than none.
Cara Hritz
January 2, 2026 AT 03:33Wait so you’re saying the FDA allows generics to vary by 45% in absorption? That’s insane. I had a friend who took generic warfarin and ended up in the ER with a brain bleed. The pharmacist said it was ‘within range.’ What range? The range where you die?!
Also, I just checked my levothyroxine bottle-different color than last month. No one told me. I didn’t notice until I started feeling dizzy. This is a disaster waiting to happen.
Adarsh Dubey
January 2, 2026 AT 11:51There’s a reason why doctors prescribe brand names even when unnecessary: they’re protecting themselves legally. If a patient has a bad outcome after a switch, the doctor could be blamed for not ‘sticking with what worked.’ So they default to brand. It’s not about money. It’s about liability.
And honestly? If you’ve been stable on a brand for years, why risk it? The cost savings are real-but so is the anxiety. Sometimes, peace of mind is worth $400.
Pankaj Chaudhary IPS
January 3, 2026 AT 19:12Replying to @6228: Your story is why we need better pharmacist training. If you had a reaction before, your pharmacy should’ve flagged it. Not assumed you didn’t care. That’s systemic failure, not bad luck.