Trimethoprim Hyperkalemia Risk Calculator
This tool estimates your risk of developing dangerous hyperkalemia (high potassium) when taking trimethoprim based on medical factors. Remember: This is for informational purposes only and does not replace medical advice.
Your estimated risk: %
Continue monitoring potassium levels as recommended by your doctor.
Your estimated risk: %
Consider discussing alternative antibiotics with your doctor. Potassium should be checked at 48-72 hours.
Your estimated risk: %
Consult your doctor immediately about safer alternatives. Potassium should be checked before and within 72 hours of starting trimethoprim.
Key Recommendations
- Check potassium before starting trimethoprim
- Get follow-up testing at 48-72 hours
- Consider alternatives: nitrofurantoin or fosfomycin
- Watch for symptoms: muscle weakness, palpitations, nausea
Most people think of antibiotics as simple fixes for infections - take a pill, feel better. But trimethoprim, a key part of the widely used antibiotic combo Bactrim or Septra, hides a dangerous secret: it can spike your potassium levels to life-threatening heights, even if you’re young and healthy.
It’s not a rare glitch. Around 8 out of every 100 people who take trimethoprim develop high potassium. That number jumps to nearly 1 in 5 if you have kidney trouble. And here’s the kicker - you might not feel a thing until your heart starts skipping beats. This isn’t theoretical. People have died from it after just three days on the drug.
How Trimethoprim Tricks Your Kidneys
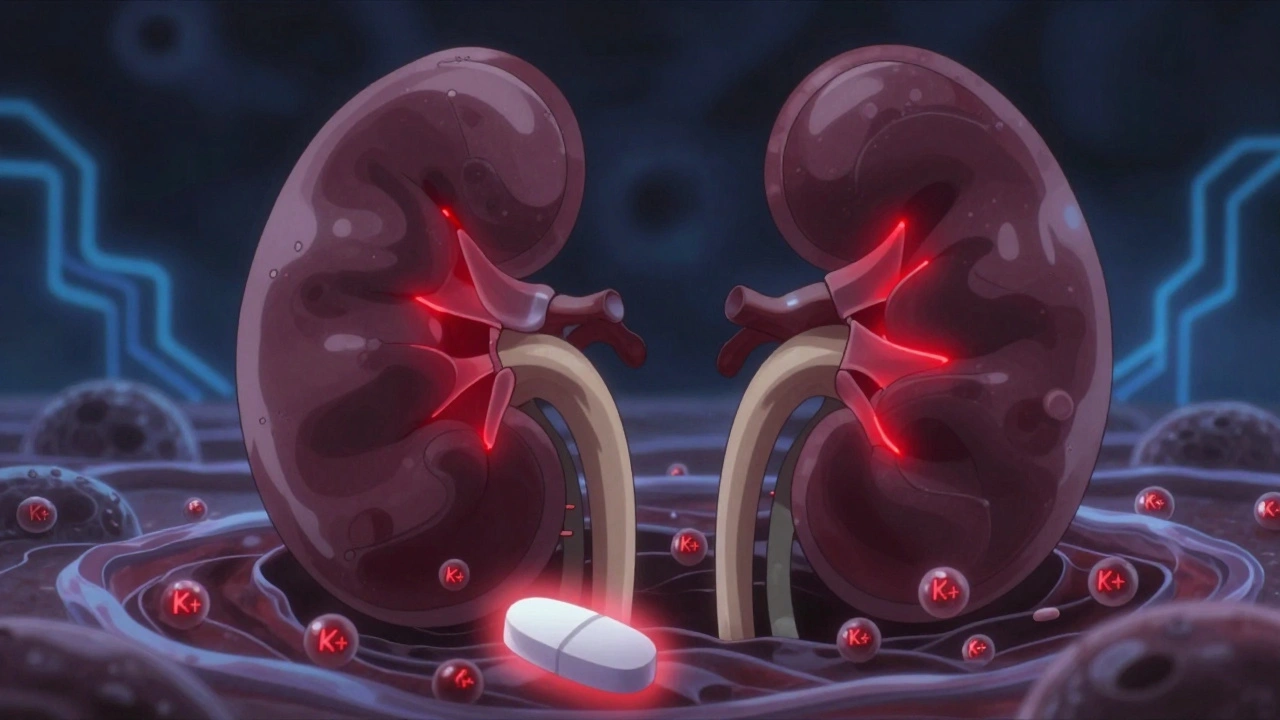
Trimethoprim doesn’t work like a typical antibiotic when it comes to potassium. It mimics a drug called amiloride - a potassium-sparing diuretic. That means it blocks tiny channels in your kidneys called ENaC, which normally help your body get rid of excess potassium through urine.
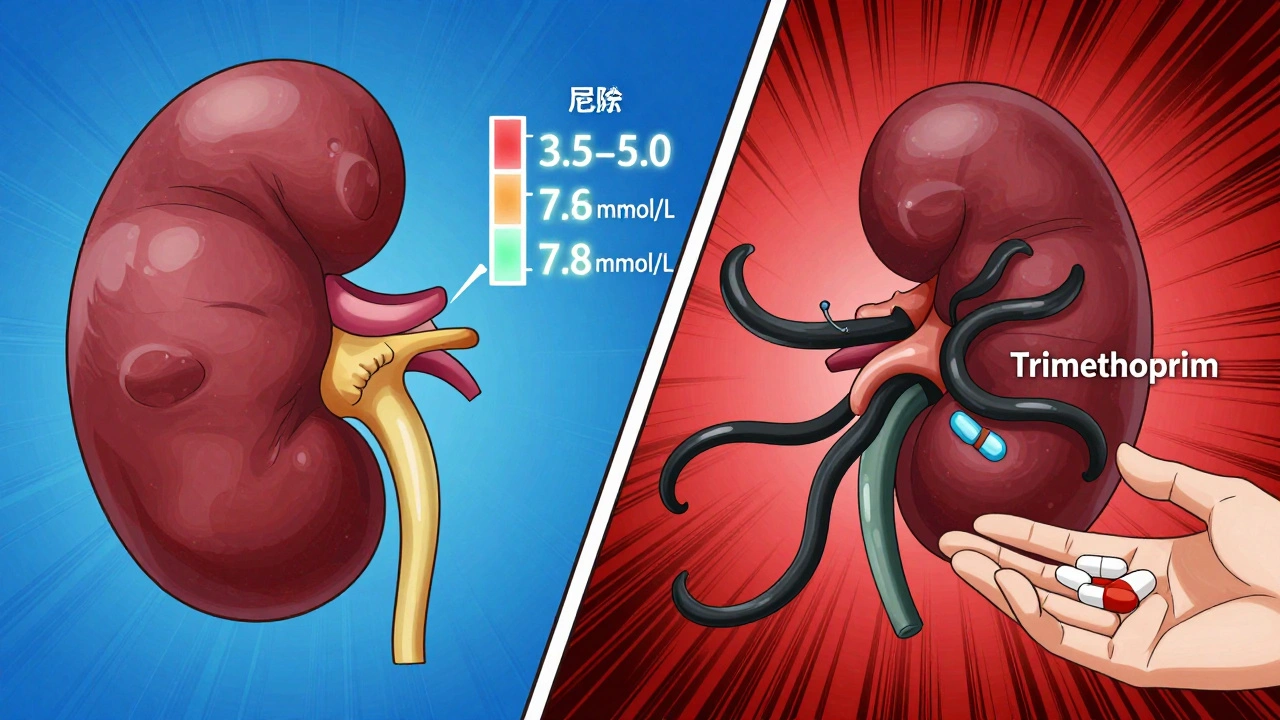
When those channels shut down, potassium stays trapped in your blood. Your kidneys stop excreting it. Even if your kidneys are otherwise fine, this blockage can raise your potassium by 0.5 to 1.5 mmol/L within just 48 to 72 hours. That might sound small, but in medical terms, it’s a red alert. Normal potassium is 3.5 to 5.0 mmol/L. Go above 5.5, and your heart rhythm is at risk. Above 6.5, you’re in emergency territory.
What makes trimethoprim so potent is that it concentrates in the kidneys at levels 10 to 50 times higher than in your bloodstream. So even a single 160/800 mg tablet - often prescribed for a urinary tract infection - can trigger this effect. A 2023 case report described an 80-year-old woman with normal kidney function who collapsed from cardiac arrest after just three days of prophylactic trimethoprim. Her potassium hit 7.8 mmol/L.
Who’s at Highest Risk?
This isn’t a risk that affects everyone equally. The biggest danger zone is for people taking medications that already raise potassium - like ACE inhibitors (lisinopril, enalapril) or ARBs (losartan, valsartan). These drugs are common for high blood pressure and heart failure, so millions of people are on them.
A major 2014 study in JAMA Internal Medicine found that older adults on ACEIs or ARBs who took trimethoprim had a 6.7 times higher chance of being hospitalized for high potassium than those who took amoxicillin. That’s not a small bump - it’s a massive spike. In fact, for every 1,000 people treated with trimethoprim in this group, about 6.6 ended up in the hospital because of potassium.
The risk skyrockets if you have three things: diabetes, chronic kidney disease (stage 3 or worse), and you’re on an ACEI or ARB. One study found that in this group, over 32% developed dangerous hyperkalemia on trimethoprim - compared to just 4% on other antibiotics.
Age matters too. People over 65 are 3 times more likely to have a severe reaction. The FDA’s own adverse event database from 2010 to 2020 showed that 68% of deaths linked to trimethoprim-induced hyperkalemia happened in patients over 65.
Why Doctors Still Prescribe It
If it’s so dangerous, why is it still everywhere? Because for some infections, it’s still the best tool.
Trimethoprim-sulfamethoxazole is the go-to for Pneumocystis pneumonia - a serious lung infection that hits people with weakened immune systems, like those with HIV or on chemotherapy. For them, the risk of dying from the infection far outweighs the risk of high potassium - if they’re monitored.
It’s also commonly used for urinary tract infections, especially when other antibiotics fail. But here’s the problem: most doctors don’t realize how fast potassium can rise. A 2023 survey found only 42% of primary care doctors check potassium levels before prescribing trimethoprim to patients on blood pressure meds. Emergency room doctors? Only 32%.
Meanwhile, nephrologists - kidney specialists - check potassium in nearly 9 out of 10 cases. That gap is deadly.

What Happens When Potassium Gets Too High
High potassium doesn’t always cause symptoms. That’s why it’s so sneaky. Some people feel nothing. Others get muscle weakness, tingling, nausea, or an irregular heartbeat. In severe cases, it can cause cardiac arrest.
When potassium hits 6.0 mmol/L or higher, doctors have to act fast. Treatment includes:
- Calcium gluconate - to stabilize the heart muscle
- Insulin and glucose - to push potassium back into cells
- Beta-agonists like albuterol - to shift potassium into cells
- Dialysis - if levels are above 7.0 or the patient has kidney failure
A 2021 review of 37 severe cases found that 43% needed emergency treatment. Most of those cases happened within 72 hours of starting the antibiotic.
Safe Alternatives Exist
You don’t have to take trimethoprim. There are safer options - especially for urinary tract infections.
Nitrofurantoin is the top alternative. Studies show it carries no increased risk of hyperkalemia. Fosfomycin is another good choice. For more serious infections, amoxicillin-clavulanate or cephalexin are often effective and don’t touch potassium levels.
The Infectious Diseases Society of America and the American Society of Health-System Pharmacists both recommend these alternatives for patients on ACEIs, ARBs, or with kidney disease - unless there’s no other option.
What You Should Do
If you’re prescribed trimethoprim, here’s what to ask for - and insist on:
- Check your potassium before you start. If it’s already above 5.0 mmol/L, ask if another antibiotic is possible.
- Get it checked again at 48-72 hours. That’s when levels peak. Don’t wait until your next appointment.
- Ask if you’re on an ACEI or ARB. If yes, and you’re over 65 or have kidney disease, question whether trimethoprim is truly necessary.
- Know the warning signs. Unexplained weakness, palpitations, or nausea after starting the drug? Call your doctor immediately.
Electronic health systems can help. Hospitals that added automated alerts - forcing doctors to check potassium before prescribing trimethoprim - cut hyperkalemia cases by over half in just one year.
The Bottom Line
Trimethoprim isn’t evil. It saves lives - especially in people with compromised immune systems. But it’s not harmless, either. It’s a hidden potassium blocker, and its risks are under-recognized.
If you’re on blood pressure meds, have kidney issues, or are over 65, don’t assume your doctor knows this risk. Ask. Push for a potassium test before and after starting the drug. If you’re not getting one, ask for an alternative.
Antibiotics aren’t all the same. Some are safe. Others? They can quietly change your chemistry - and stop your heart.
Can trimethoprim cause high potassium even if my kidneys are fine?
Yes. Even people with normal kidney function can develop dangerous hyperkalemia from trimethoprim. A 2023 case report described an 80-year-old woman with normal creatinine levels who suffered cardiac arrest after just 72 hours on the drug. Trimethoprim concentrates in the kidneys and directly blocks potassium excretion, regardless of overall kidney health.
How soon after starting trimethoprim does potassium rise?
Potassium levels typically begin rising within 24 hours and peak between 48 and 72 hours after starting the medication. Most severe cases - where potassium exceeds 6.0 mmol/L - occur within this 3-day window. Waiting until your next routine blood test can be too late.
Is nitrofurantoin safer than trimethoprim for UTIs?
Yes. Nitrofurantoin is the preferred alternative for urinary tract infections in patients on ACE inhibitors, ARBs, or with kidney disease. Multiple studies show it carries no increased risk of hyperkalemia, unlike trimethoprim, which raises potassium levels in up to 17.6% of high-risk patients. Guidelines from the Infectious Diseases Society of America recommend nitrofurantoin as first-line for uncomplicated UTIs in at-risk populations.
Should I stop taking trimethoprim if I’m on lisinopril?
Don’t stop abruptly - talk to your doctor. But if you’re on lisinopril (or any ACEI/ARB), especially if you’re over 65 or have kidney disease, you should ask whether trimethoprim is truly necessary. The risk of hyperkalemia is 6.7 times higher than with safer antibiotics like amoxicillin. Alternatives like nitrofurantoin or fosfomycin are available and much safer for your potassium levels.
Do all antibiotics raise potassium levels?
No. Trimethoprim is one of the few antibiotics known to directly interfere with potassium excretion. Most others - like amoxicillin, cephalexin, or ciprofloxacin - don’t affect potassium. Even other sulfa drugs like sulfamethoxazole alone (without trimethoprim) don’t carry this risk. It’s the trimethoprim component that’s the problem.
Siddharth Notani
December 4, 2025 AT 00:58Trimethoprim is a silent killer in plain sight. I’ve seen three elderly patients on lisinopril crash within days of being prescribed Bactrim. No symptoms. No warning. Just ECG changes and cardiac arrest. Always check K+ before prescribing - it’s not optional, it’s basic.
Akash Sharma
December 4, 2025 AT 13:40I’ve been reading up on this for weeks now because my dad’s on lisinopril and got a script for trimethoprim last month for a UTI. I didn’t know this was even a thing. I mean, I knew antibiotics weren’t all harmless, but this? This is wild. He’s 71, kidney function’s okay but not perfect, and his potassium was 5.2 last check - borderline high. I called his GP and they were like, ‘Oh, we didn’t think it was a big deal.’ I’m now demanding a repeat K+ before he takes a single pill. This isn’t just a medical footnote - it’s a ticking time bomb for millions. And why isn’t there an automated alert in every EHR? Why do we still rely on doctors remembering? We’ve got the tech. We’ve got the data. This should be locked in like a drug interaction warning for warfarin. It’s not a ‘maybe,’ it’s a ‘definitely.’
Justin Hampton
December 5, 2025 AT 02:27So let me get this straight - you’re scared of a 17% risk in high-risk groups but ignore that 80% of people take it without issue? You’re pathologizing a common antibiotic because some doctors are lazy. Next you’ll say aspirin causes bleeding so we should ban it. Wake up.
Pooja Surnar
December 5, 2025 AT 03:12Sandridge Nelia
December 6, 2025 AT 14:35This is exactly why I always ask for a basic metabolic panel before any new antibiotic if I’m on blood pressure meds. I’m 68, on lisinopril, and I refuse to take anything without checking K+ first. My doctor used to roll her eyes - now she thanks me. Seriously, if you’re over 60 and on an ACEI/ARB, this is non-negotiable. Don’t be brave. Be smart. 💪❤️
Mark Gallagher
December 8, 2025 AT 09:18It’s embarrassing that this is even a debate. In the U.S., we have the best medical infrastructure in the world - yet we’re still letting doctors prescribe life-threatening drugs without mandatory labs. This isn’t a ‘risk,’ it’s negligence. And it’s worse in countries like India where people self-medicate with Bactrim from pharmacies. This isn’t a medical issue - it’s a systemic failure of accountability.
Wendy Chiridza
December 9, 2025 AT 08:23I’m a nurse and I’ve seen this too many times. Patient comes in with palpitations, potassium 7.9, just started trimethoprim for a UTI. No one checked. No one asked. They were prescribed it because it’s cheap and easy. Nitrofurantoin costs the same. Fosfomycin is one pill. Why are we still doing this? We need mandatory alerts in the EHR. Period.
Pamela Mae Ibabao
December 11, 2025 AT 00:45Oh honey, I love how you say 'trimethoprim isn’t evil' - like it’s some misunderstood villain in a Disney movie. It’s not evil, it’s just a chemical that doesn’t care if you live or die. And doctors? They’re not villains either - they’re just overwhelmed, overworked, and undertrained on this specific risk. But here’s the thing: the fact that 68% of deaths are in patients over 65? That’s ageism disguised as medical practice. We don’t test elderly patients for this because we assume they’ll die anyway. And that’s the real tragedy.
Gerald Nauschnegg
December 11, 2025 AT 05:32Wait wait wait - so you’re telling me that a drug I took last year for a bladder infection could’ve killed me? I’m 52, no kidney issues, no BP meds - but I did have a weird tingling in my fingers after day two. Thought it was anxiety. You’re telling me that was potassium? Holy crap. I’m going to get my labs done tomorrow. This is terrifying. Thank you for posting this. I didn’t even know to ask.
Palanivelu Sivanathan
December 12, 2025 AT 05:31Joanne Rencher
December 12, 2025 AT 16:28Erik van Hees
December 13, 2025 AT 08:27Let’s be real - this isn’t about trimethoprim. It’s about how medicine is still stuck in the 1990s. We’ve got AI, real-time monitoring, and predictive analytics - yet we’re still relying on doctors to remember a single drug interaction that’s been known since 2010? The FDA should mandate EHR alerts for trimethoprim + ACEI/ARB + age >65. If a system doesn’t auto-flag it, it shouldn’t be allowed to prescribe. This isn’t a suggestion. It’s a damn requirement. And if your EHR doesn’t do it, switch hospitals. Your life isn’t a beta test.