Understanding Postherpetic Neuralgia and Chronic Fatigue Syndrome
Before diving into the connection between postherpetic neuralgia (PHN) and chronic fatigue syndrome (CFS), it is important to understand what these two medical conditions are. Postherpetic neuralgia is a painful complication of shingles, which is caused by the same virus responsible for chickenpox. PHN occurs when nerve fibers are damaged during the shingles outbreak, leading to persistent nerve pain that can last for months or even years after the rash has healed.
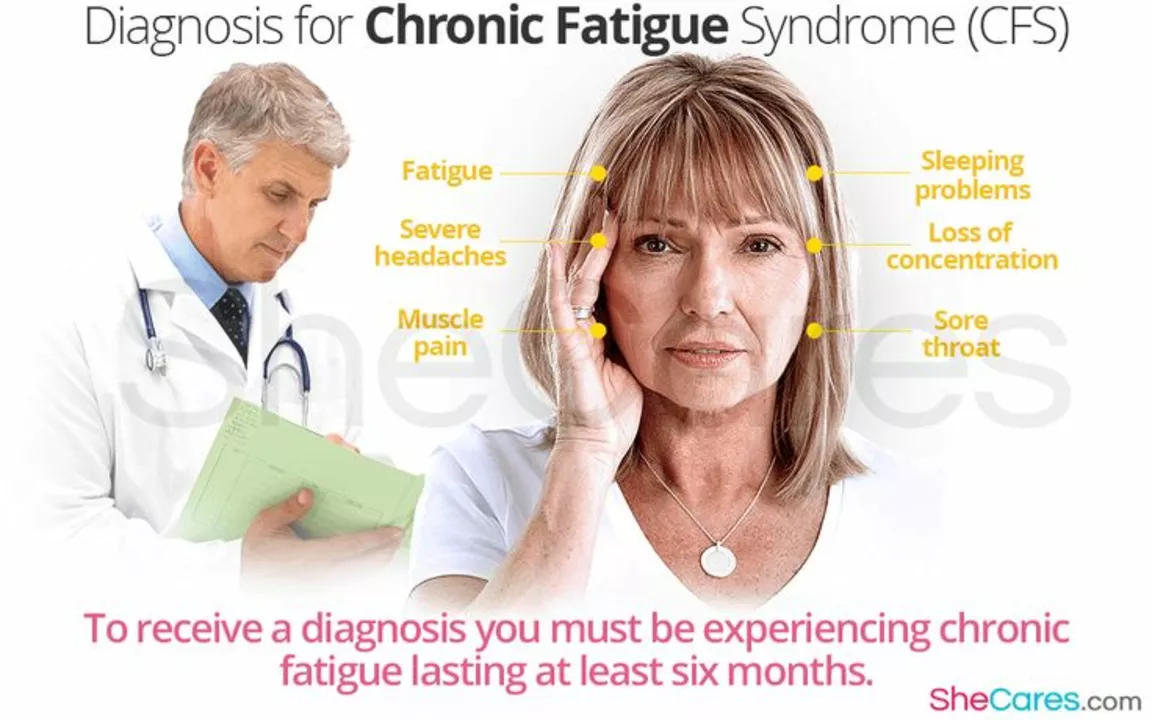
Chronic fatigue syndrome, on the other hand, is a complex and debilitating disorder characterized by extreme tiredness that cannot be explained by any underlying medical condition. The fatigue experienced by individuals with CFS is not improved by rest and can worsen with physical or mental activity. Although the exact cause of CFS remains unknown, various factors such as viral infections, immune system problems, and hormonal imbalances have been suggested as possible triggers.
The Shared Symptoms of PHN and CFS
Though postherpetic neuralgia and chronic fatigue syndrome are distinct medical conditions, they share some common symptoms. Both PHN and CFS can present with persistent pain, which can be severe and disabling in some cases. Additionally, individuals with either condition may experience sleep disturbances, difficulties concentrating, and mood changes such as depression or anxiety.
These overlapping symptoms can make it challenging for healthcare providers to differentiate between PHN and CFS, particularly when a patient has a history of shingles. A thorough evaluation of the patient's medical history, symptoms, and physical examination is crucial for an accurate diagnosis and appropriate treatment plan.
Exploring the Connection Between PHN and CFS
Although the exact relationship between postherpetic neuralgia and chronic fatigue syndrome is still not fully understood, some researchers believe there may be a connection. One possible explanation is that the virus that causes shingles, the varicella-zoster virus (VZV), may also play a role in the development of CFS. Some studies have found a higher prevalence of VZV antibodies in individuals with CFS, suggesting a possible link between the two conditions.
Another possibility is that the chronic pain and discomfort associated with PHN can contribute to the development of CFS in some individuals. Chronic pain can lead to sleep disturbances, reduced physical activity, and increased stress levels, all of which are known risk factors for CFS. Furthermore, the immune system dysregulation seen in CFS may be triggered by the persistent inflammation associated with PHN.
Managing Pain and Fatigue in PHN and CFS
Regardless of the exact connection between postherpetic neuralgia and chronic fatigue syndrome, managing pain and fatigue is essential for improving the quality of life for individuals living with these conditions. Pain management strategies for PHN may include medications such as anticonvulsants, antidepressants, or opioids, as well as non-pharmacological approaches like nerve blocks, physical therapy, or transcutaneous electrical nerve stimulation (TENS).
For those with CFS, treatment typically focuses on managing individual symptoms and may include medications to address pain, sleep disturbances, and mood changes. Additionally, lifestyle modifications such as pacing activities, maintaining a regular sleep schedule, and engaging in gentle exercise can help to manage fatigue and improve overall function.
Seeking Support for PHN and CFS
Living with postherpetic neuralgia or chronic fatigue syndrome can be challenging, both physically and emotionally. It is important for individuals with these conditions to seek support from healthcare providers, family, friends, and support groups. Connecting with others who share similar experiences can provide valuable insights, coping strategies, and encouragement for managing the daily challenges of living with PHN or CFS.
In conclusion, while the exact connection between postherpetic neuralgia and chronic fatigue syndrome remains unclear, it is evident that individuals with either condition can benefit from similar management strategies and support systems. By understanding the potential link between these two conditions and working closely with healthcare providers, individuals with PHN or CFS can take steps to manage their symptoms and improve their overall quality of life.
Karen Werling
May 1, 2023 AT 07:40Just wanted to say: you're not crazy. This is real.
Billy Gambino
May 2, 2023 AT 01:51Studies by Peterson et al. (2021) demonstrate elevated CSF IL-6 and TNF-alpha in PHN patients who later developed CFS-like phenotypes. The viral latency-reservoir hypothesis is gaining traction, particularly with recent single-cell RNAseq data implicating latent VZV in autonomic nervous system dysfunction.
STEVEN SHELLEY
May 2, 2023 AT 09:45Emil Tompkins
May 2, 2023 AT 22:12Also, why is everyone acting like CFS is some mysterious alien illness? It's just burnout with a fancy name. People need to stop being so fragile. I don't need a 10-page paper to tell me pain makes you tired.
Kevin Stone
May 3, 2023 AT 13:48Stop looking for external causes. Look in the mirror. Your lifestyle is your diagnosis.
STEVEN SHELLEY
May 4, 2023 AT 07:58