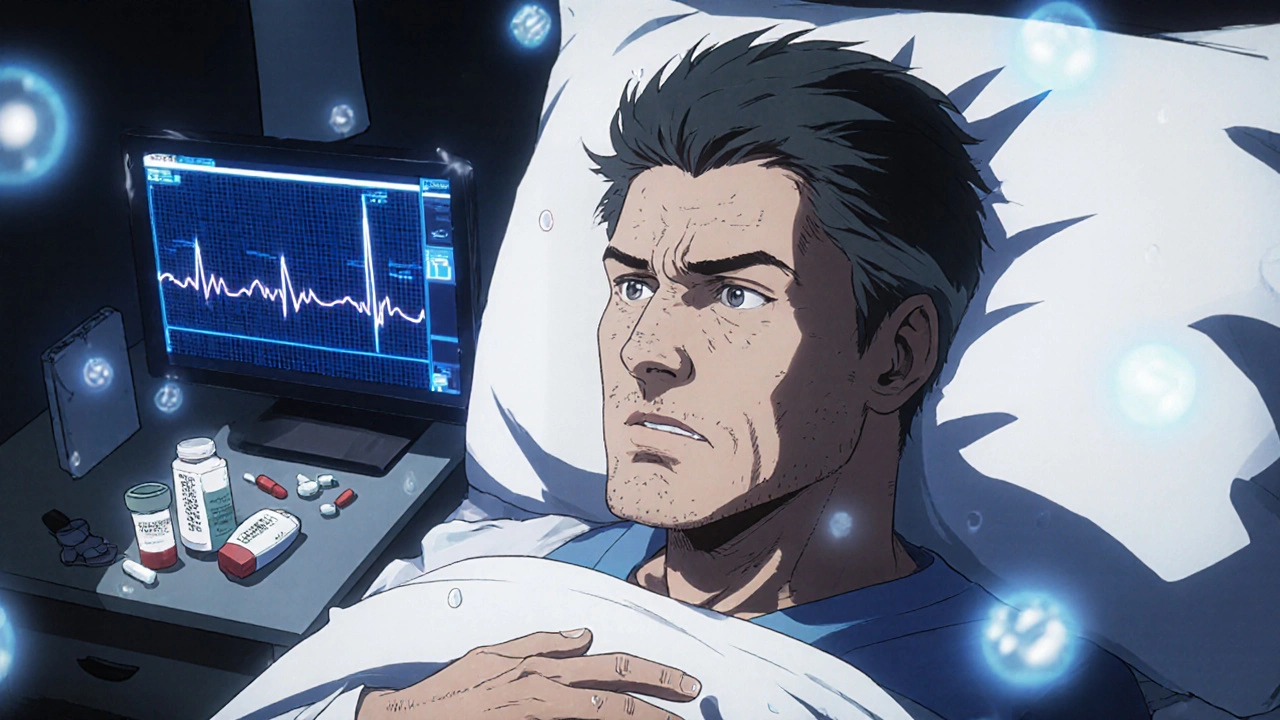
Medication-Induced Arrhythmia: Risks, Triggers, and How to Stay Safe
When a drug changes your heart’s rhythm, it’s not just a side effect—it’s a serious risk. Medication-induced arrhythmia, an abnormal heart rhythm triggered by prescription or over-the-counter drugs. Also known as drug-induced arrhythmia, it can turn a routine medication into a life-threatening event. This isn’t rare. It happens when a drug interferes with the electrical signals that keep your heart beating steady. Some medications slow down or speed up these signals just enough to cause chaos—like a short circuit in a heart that’s otherwise healthy.
One of the biggest culprits is QT prolongation, a delay in the heart’s electrical recovery phase that can lead to dangerous rhythms like torsades de pointes. Drugs like certain antipsychotics, medications used to treat schizophrenia and bipolar disorder, and even some antibiotics or nausea drugs can trigger it. Combine them with other QT-prolonging meds, and the risk spikes. That’s why doctors check your full list of meds before prescribing—even if you’re just taking an OTC sleep aid or herbal supplement. Blood thinners, like warfarin or rivaroxaban, aren’t usually linked to arrhythmias directly, but they often appear in the same patient profiles as drugs that are. People on multiple meds for heart disease, depression, or chronic pain are at higher risk—not because any single drug is dangerous, but because of how they stack up.
It’s not just about the pills you take. It’s about what you mix them with. Turmeric, kava, or even high-dose vitamin B6 can quietly interfere with how your heart handles medication. And if you’re older, have kidney or liver issues, or are female, your body processes these drugs differently—making you more sensitive to their effects. You might not feel anything until your heart skips a beat, then races, then nearly stops. That’s when it’s too late.
What you need isn’t fear—it’s awareness. If you’re on any of these drugs, know the signs: dizziness, palpitations, sudden shortness of breath, or fainting. Get an EKG if your doctor suggests it. Ask if your meds are on the QT prolongation list. Don’t assume natural means safe. And never stop a prescription cold turkey—talk to your pharmacist or doctor first. Below, you’ll find real cases and clear guides on which medications carry the highest risk, how to monitor for trouble, and what alternatives exist that won’t put your heart in danger.
Heart Arrhythmias from Medications: Warning Signs and How to Manage Them
Over 400 common medications can trigger dangerous heart rhythm problems. Learn the warning signs - like palpitations, dizziness, and fainting - and how to manage drug-induced arrhythmias safely before they become life-threatening.
learn more