Joint Pain Genetics: How Your DNA Affects Arthritis and Chronic Discomfort
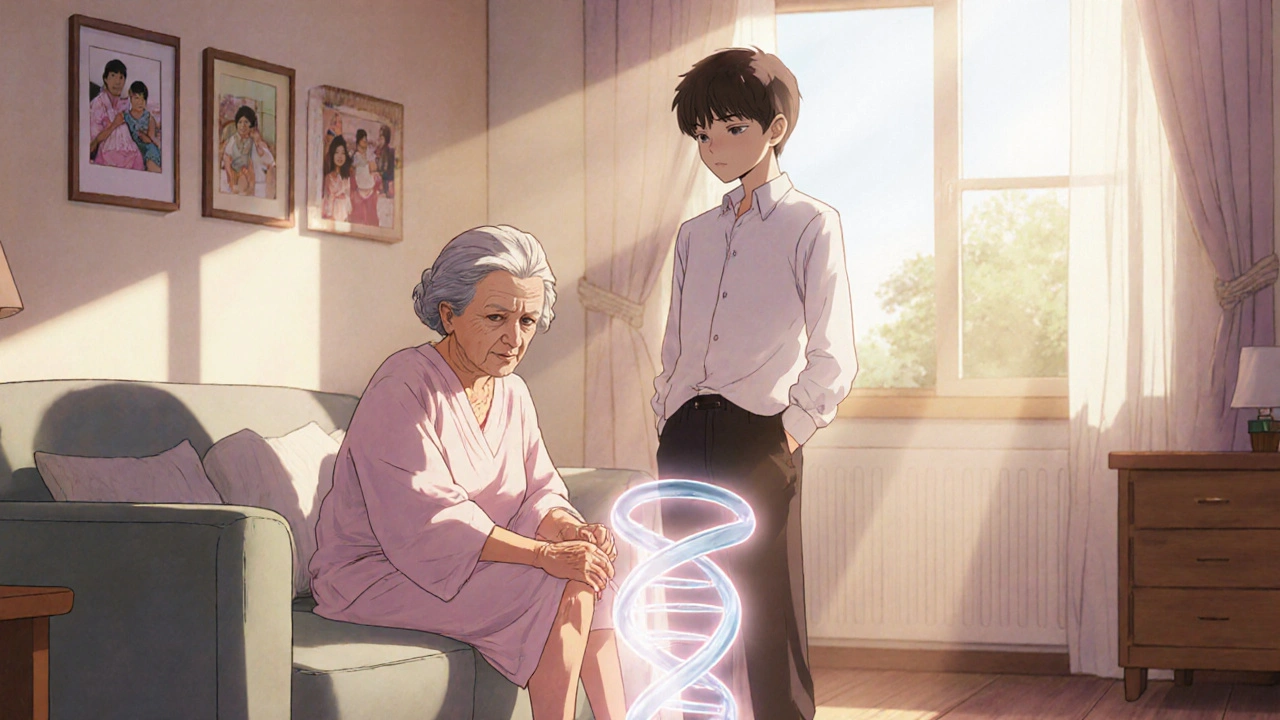
When your knees ache, your hands stiffen, or your hips refuse to move without a protest, it’s easy to blame age, weather, or overuse. But what if the real culprit is hiding in your DNA? Joint pain genetics, the inherited biological factors that determine how your joints respond to wear, inflammation, and injury. Also known as genetic predisposition to arthritis, it’s not just about getting older—it’s about how your body was built from the start. Studies show that up to 60% of osteoarthritis cases and nearly 50% of rheumatoid arthritis cases have a strong genetic component. If your mom or dad had bad knees before 50, you’re not just unlucky—you might have inherited the same gene variants that make cartilage break down faster or immune cells attack joint tissue.
It’s not one gene that causes joint pain. It’s a mix. The COL2A1 gene, a key builder of cartilage structure, has mutations linked to early-onset osteoarthritis. Then there’s the HLA-DRB1 gene, a major player in immune system behavior, which can turn your body’s defenses against your own joints, triggering rheumatoid arthritis. And don’t forget FTO gene variants, linked to body weight and fat distribution—extra weight doesn’t just strain joints, it also changes how your body produces inflammatory chemicals. These genes don’t guarantee pain, but they tilt the odds. Someone with the right combination might develop joint issues in their 30s, while a neighbor with the same lifestyle stays pain-free into their 70s.
Knowing your genetic risk doesn’t mean you’re doomed. It means you can act earlier. If your family history shows early joint problems, getting checked before symptoms hit—maybe with a simple blood test or joint imaging—can catch trouble before it escalates. Lifestyle changes like low-impact exercise, anti-inflammatory diets, and weight control become even more powerful when you know your genes are working against you. And yes, some of the medications you’ve seen in our posts—like Etodolac for spinal stenosis pain or calcitonin for bone discomfort—are used not just to treat symptoms, but to slow damage in people with high genetic risk. You’re not just managing pain. You’re fighting a hidden battle coded into your cells.
Below, you’ll find real comparisons of medications, treatments, and lifestyle strategies that actually help people with inherited joint issues—not just theory, but what works today. Some posts dive into painkillers that ease inflammation. Others look at how genetics shape who responds best to certain drugs. You’ll see how people with similar DNA profiles are managing their pain, avoiding surgery, and staying active. This isn’t about guessing. It’s about using what science knows about your genes to make smarter choices.
Is Joint Pain Hereditary? Genetics and Joint Pain Explained
Explore how genetics influence joint pain, learn to spot hereditary patterns, and discover practical ways to manage risk and reduce discomfort.
learn more