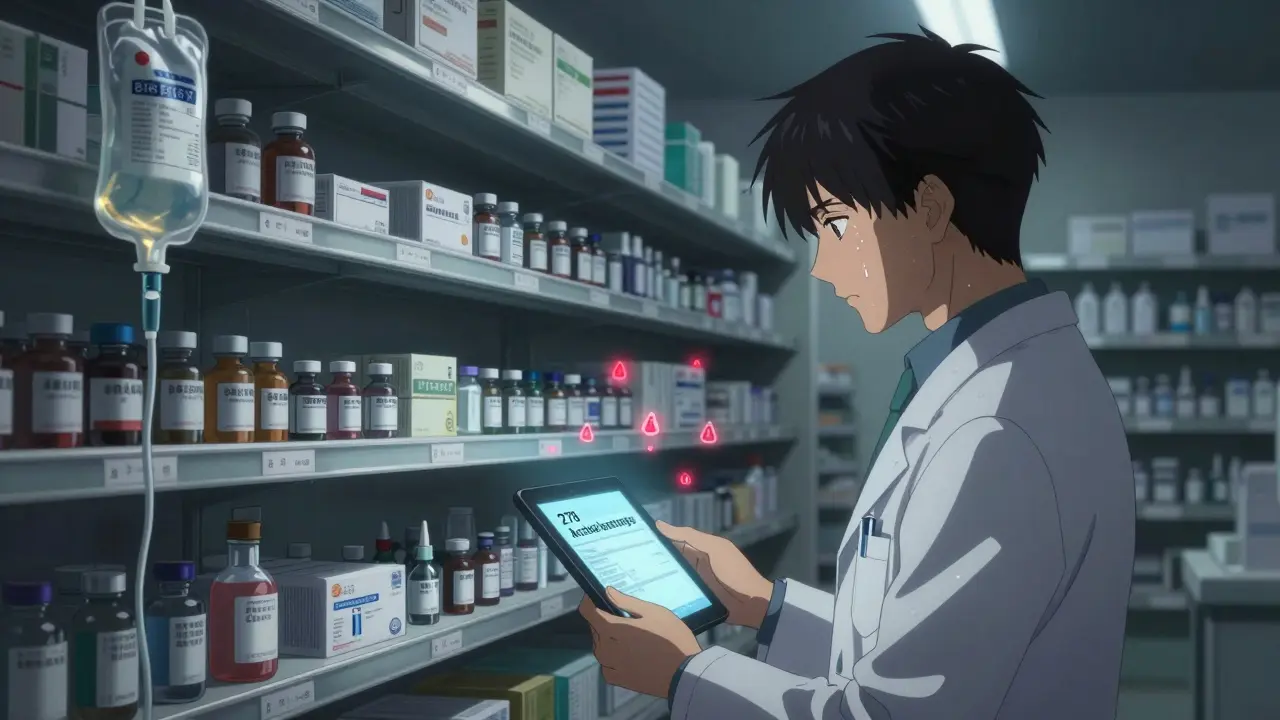
By now, most people know that generic drugs are cheaper. But few realize how fragile their supply really is. In April 2025, there were 270 active drug shortages in the U.S., and nearly all of them were generic medications. These aren’t obscure pills. These are life-saving drugs like IV fluids, chemotherapy agents, antibiotics, and epinephrine - the kind you rely on in a hospital, an ER, or even at home. When they disappear, the system doesn’t just slow down. It breaks.
Why Generic Drugs Are the First to Go
Generic drugs make up 90% of all prescriptions filled in the U.S. But they account for just 13.1% of total drug spending. That math doesn’t add up - unless you understand the business behind it. Generic manufacturers operate on razor-thin margins. A single vial of a generic antibiotic might cost less than $2. To stay profitable, companies must produce thousands of doses at ultra-low cost. That means cutting corners where they can - and relying on the cheapest suppliers possible. The biggest cut? Manufacturing. Less than 30% of active pharmaceutical ingredients (APIs) used in American drugs are made in the U.S. The rest come from just two countries: China and India. China alone supplies about 40% of the world’s APIs. That’s not just a supply chain. It’s a single point of failure. When a factory in India gets shut down by the FDA for quality violations - like what happened with cisplatin, a key chemotherapy drug - there’s no backup. There’s no extra inventory. There’s no alternative source. And because no one’s making a profit on that drug, no one rushes to replace it.Sterile Injectables: The Most Vulnerable
Not all generic drugs are created equal. Oral pills are simple to make. But sterile injectables - the ones given through IVs - are a whole different challenge. They require clean rooms, specialized equipment, and hours of precision. One tiny mistake, and the whole batch is contaminated. That’s why these drugs are the most common in shortage lists. Think about it: you can’t just swap out an IV bag of saline for a different one. You can’t substitute a chemotherapy drug without risking patient safety. In 2023, a tornado destroyed a Pfizer plant that made 15 different critical medications. That wasn’t a natural disaster. It was a supply chain collapse. And because those drugs had only one or two manufacturers, the entire country felt the impact. The FDA has documented over 20 essential drugs that teetered on the edge of shortage during the pandemic. Most were sterile injectables. And the problem didn’t start with COVID. It started decades ago, when manufacturers moved production overseas to save money - and nobody built a safety net.The Single-Point Failure Problem
For many generic drugs, manufacturing has shrunk to just one or two companies. If one of them has a quality issue, shuts down for repairs, or gets hit by a political or natural disaster, the drug vanishes. There’s no competition. No backup. No alternative. Take heparin, a blood thinner used in surgeries and dialysis. For years, it was made by just one company in China. When quality issues arose, the FDA paused imports. Hospitals scrambled. Patients faced delays. Some had to go without. This isn’t rare. The USP Annual Drug Shortage Report found that for nearly half of all shortage drugs, only one manufacturer remains. That’s not market competition. That’s market collapse.
Why Tariffs Won’t Fix This
Some politicians say the answer is tariffs - slap a 50% or even 200% tax on drugs made overseas to force production back to the U.S. But that’s like trying to fix a leaky boat by throwing more weight into it. Tariffs raise the cost of APIs. That raises the cost of the final drug. But generic manufacturers can’t raise prices. They’re locked into contracts with hospitals and insurers that pay fixed, low rates. So what happens? They stop making the drug. The shortage gets worse. The CSIS analysis warns that tariffs could lead to “higher costs, delayed treatment, and increased shortages” - exactly the opposite of what’s intended. And it’s not just about money. Rebuilding domestic manufacturing takes five to seven years and $20-30 billion. That’s not a policy fix. That’s a national project.What’s Really Happening Behind the Scenes
Pharmacists are the ones on the front lines. One hospital pharmacist told Pharmacy Times they spend 20-30% of their workweek just managing shortages. That’s not filling prescriptions. That’s calling suppliers, compounding drugs from scratch, rationing doses, and convincing doctors to switch to riskier alternatives. Hospitals have started stockpiling. But they can’t stockpile everything. A single IV bag of saline lasts a few hours. A chemotherapy drug might be needed once a week. You can’t keep a six-month supply of every critical drug on hand. And even if you could, the cost would bankrupt the system. Patients feel it too. Cancer treatments get delayed. Surgeries get canceled. Antibiotics run out. People are being told to wait - sometimes for weeks - because the drug they need isn’t available.
What Could Actually Help
There are no easy answers. But some ideas are starting to gain traction. One is the Strategic National Stockpile - but expanded. Right now, it holds mostly vaccines and emergency supplies. Experts are pushing to add critical generic injectables. Imagine having a federal reserve of essential drugs, ready to deploy when a factory shuts down. Another idea: require manufacturers to keep a six-month supply of high-risk drugs on hand. That’s what S.2062 proposes. It’s not perfect. It’s expensive. But it’s better than waiting for disaster to strike. Transparency matters too. Right now, you can’t tell if your generic drug was made in China, India, or the U.S. Requiring clear labeling on API origin would let regulators, hospitals, and even patients see where the risk lies. And finally - we need more manufacturers. Not just one or two. Dozens. If 10 companies make the same generic drug, one factory closing won’t cause a crisis. But right now, economic incentives are stacked against new entrants. Low prices mean low profits. No profit means no investment. No investment means no new factories.The Bigger Picture
The problem isn’t just about drugs. It’s about how we value health. We treat generic medications like commodities - cheap, replaceable, disposable. But when you’re the patient on the other end, they’re not commodities. They’re survival. We’ve built a system that depends on global suppliers, thin margins, and zero redundancy. And when things break - and they will - it’s patients who pay the price. The next time you hear about a drug shortage, don’t think it’s just a supply issue. Think of the hospital pharmacist working 12-hour shifts. The cancer patient waiting for treatment. The ER doctor choosing between two risky alternatives. This isn’t a problem that will solve itself. It needs policy. Investment. And a shift in how we see the most basic medicines we rely on every day.Why are generic drug shortages getting worse?
Generic drug shortages are worsening because manufacturing has become dangerously concentrated in just a few countries - mainly China and India - and only one or two companies typically make each drug. Low profit margins mean manufacturers have little incentive to invest in quality, backup production, or inventory. When one factory shuts down due to quality issues, natural disasters, or political disruptions, there’s no backup, and no one rushes to fill the gap.
Are brand-name drugs affected by shortages too?
Brand-name drugs are less affected because their manufacturers have higher profit margins, which let them maintain larger inventories, diversify suppliers, and absorb disruptions like tariffs or quality issues. They also invest in multiple production sites and flexible manufacturing. Generic drugs, by contrast, are priced so low that companies can’t afford those safeguards.
Can the U.S. just make all generic drugs domestically?
Rebuilding full domestic production for generic drugs would take 5-7 years and cost $20-30 billion. It’s technically possible, but economically unrealistic. Most generic drugs sell for pennies per dose, and no company will invest billions into a market that doesn’t pay enough to return a profit. A better approach is targeted domestic production for critical drugs - like IV fluids and chemotherapy agents - not everything.
How do drug shortages affect patient care?
Shortages force doctors to use less effective or riskier alternatives. Patients delay cancer treatments, surgeries get canceled, and antibiotics run out during outbreaks. One hospital pharmacist reported patients being told to wait weeks for essential medications. In extreme cases, shortages have led to preventable deaths - especially in intensive care and oncology units.
What role does the FDA play in drug shortages?
The FDA inspects foreign manufacturing facilities and can shut down production if quality standards aren’t met. But it has fewer inspectors for overseas sites than domestic ones. Meanwhile, U.S. inspection capacity has been reduced due to budget cuts. This creates gaps where unsafe products slip through - and then disappear from shelves when recalled.
Are there any current policy solutions being considered?
Yes. Congress is considering bills like S.2062, which would require manufacturers to maintain six-month reserves of critical generic drugs. Other proposals include public-private partnerships to fund domestic production, mandatory API labeling, and expanding the Strategic National Stockpile to include essential injectables. But progress is slow due to political gridlock and underfunded federal agencies.