Shoulder pain doesn’t just come and go-it steals your sleep, ruins your workouts, and makes even simple tasks like reaching for a coffee mug feel impossible. If you’ve been told you have rotator cuff issues or bursitis, you’re not alone. Over 2 million Americans visit doctors each year for shoulder pain tied to these exact problems. And here’s the truth: most of them don’t need surgery. What they need is the right rehab plan, done right.
What’s Really Going On in Your Shoulder?
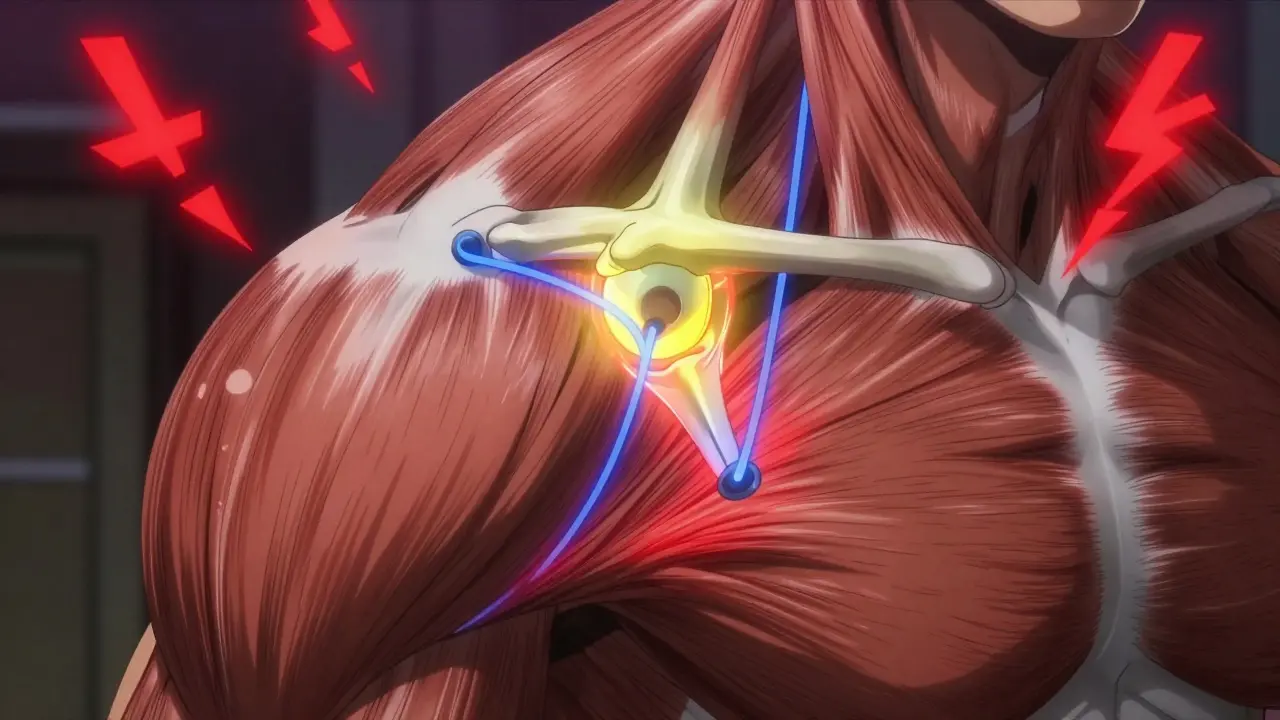
Your shoulder is a ball-and-socket joint, but unlike your hip, it’s not locked in place. It’s held together by four small muscles-the supraspinatus, infraspinatus, teres minor, and subscapularis-that form the rotator cuff. These muscles don’t move your arm; they keep the ball centered in the socket when you lift, reach, or throw. When they get overworked or irritated, they swell. That’s tendinitis. Right above them is a fluid-filled sac called the subacromial bursa. Its job? To reduce friction between the tendons and the bony shelf above them (the acromion). When the tendons rub too much, the bursa gets inflamed-that’s bursitis. The two often happen together. Think of it like a car engine with worn parts and a leaking gasket. One problem makes the other worse. The classic sign? The painful arc. When you lift your arm out to the side, between 60 and 120 degrees, it hurts. That’s because that’s the exact spot where the inflamed tissues get pinched. Pain at night, especially when lying on the shoulder, is another red flag. Around 78% of patients report sleep disruption in the early stages, according to Cedars-Sinai’s 2023 patient survey.How Doctors Diagnose It (And Why Imaging Isn’t Always the Answer)
Most orthopedic doctors start with a physical exam. They’ll move your arm in specific ways to see where pain hits. They’ll check your strength, range of motion, and whether your shoulder blade moves abnormally-a sign of scapular dyskinesis, which is often the hidden cause. Imaging? It’s helpful, but overused. Ultrasound can show if the bursa is swollen past 2 mm (normal is under 1 mm). MRI can spot tears in the rotator cuff tendons. But here’s the catch: many people over 50 have rotator cuff tears on MRI and feel zero pain. Meanwhile, someone with intense pain might have a perfectly normal scan. That’s why diagnosis isn’t about the image-it’s about your symptoms, your movement, and your history.What Actually Helps? The Real Rehab Protocol
Forget resting for weeks. That’s outdated. The modern approach starts with movement-gentle, controlled movement-within 48 hours of pain starting.- Pendulum exercises: Lean over, let your arm hang, and gently swing it in small circles. Do this 5-10 minutes, three times a day. This keeps the joint lubricated and prevents stiffness.
- Active-assisted motion: After 2-3 weeks, use your good arm to help the painful one lift overhead, using a broomstick or towel. No force. Just smooth motion.
- Scapular retraction: Squeeze your shoulder blades together like you’re trying to hold a pencil between them. Hold for 5 seconds, repeat 15 times, three sets a day. Patients who do this consistently see pain resolve 30% faster than those who only focus on rotator cuff exercises.
- Resistance band work: At 4-6 weeks, start light strengthening with a TheraBand. External rotation (pulling band away from your body), internal rotation (pulling toward your belly), and scaption (raising arm slightly forward at 30 degrees) are the big three. Do 15-20 reps per set, two to three times a week. Keep the resistance at 30-50% of your max effort.

When Injections Make Sense (And When They Don’t)
If you’ve tried 4-6 weeks of rehab and still can’t sleep or lift your arm, a corticosteroid injection might help. It’s not a cure-it’s a reset button. The injection, usually 1-2 mL of triamcinolone acetonide mixed with lidocaine, goes into the subacromial space under ultrasound guidance. Accuracy matters. With newer systems like AcuNav V, doctors now hit the target 94% of the time, down from 72% just a few years ago. About 65-75% of patients get relief for 4-12 weeks. That’s enough time to get into rehab and build strength without pain holding you back. But here’s the catch: don’t get more than 2-3 injections a year. Too many weaken the tendon. The risk of a full tear jumps to 8% with frequent shots. And no, PRP (platelet-rich plasma) isn’t magic. It’s a second-line option after steroids fail. A 2024 multi-center trial showed a 68% success rate for PRP versus 52% for repeat steroids. But it’s expensive, often not covered by insurance, and still being studied. Don’t fall for the hype.When Surgery Is Actually Needed
Surgery isn’t the default. In fact, 80% of rotator cuff tendinitis and bursitis cases improve without it, as long as patients stick to rehab. Surgery is considered only after 3-6 months of consistent non-surgical treatment. The most common procedure is arthroscopic subacromial decompression. The surgeon shaves down part of the acromion and removes the inflamed bursa. It’s minimally invasive-three tiny incisions, 45-60 minutes, same-day discharge. But here’s the kicker: a 2022 study in the Journal of Bone and Joint Surgery found no real difference in outcomes between surgery and intensive physical therapy at the 12-month mark. If you don’t have a full-thickness tear, surgery doesn’t give you a better result. It just gives you scars and a longer recovery. The only clear surgical candidates? People over 60 with complete rotator cuff tears. Their natural healing rate is only 40% with rehab. Surgery bumps that to 75%. For partial tears? Stick with therapy.Why Most People Fail (And How to Avoid It)
The biggest reason rehab fails? Inconsistency. Patients who use smartphone apps with exercise reminders complete 82% of their assigned workouts. Those without apps? Only 54%. That’s a 27% faster recovery just from using a calendar alert. Another big mistake? The weekend warrior effect. Someone does rehab all week, then plays golf or lifts weights on Saturday and is back in pain on Monday. That’s why 35% of repeat visits happen. Recovery isn’t linear. You can’t rush it. And don’t skip the scapular work. Most people focus only on the rotator cuff. But if your shoulder blade doesn’t move right, your tendons will keep getting pinched. Scapular control is the foundation. Without it, everything else is temporary.
What You Can Do Right Now
If you’re in pain today:- Ice your shoulder 15-20 minutes, 3-4 times a day for the first 3 days.
- Take ibuprofen 400-600 mg three times a day with food (if you can tolerate it).
- Stop overhead lifting, reaching behind your back, or sleeping on that side.
- Start pendulum exercises today-even if it’s just for 5 minutes.
- Find a physical therapist who specializes in shoulders. Ask if they use standardized protocols like the AAOS guidelines.
What’s Changing in 2026
The shoulder rehab field is evolving fast. Medicare now pays 4.7% more for supervised physical therapy and 2.3% less for steroid injections. That’s pushing clinics to start rehab earlier. New wearable sensors are being tested to give real-time feedback on your form during exercises. One company in California just got FDA clearance for a shoulder strap that vibrates if you’re shrugging your shoulder during a band exercise. It’s not mainstream yet-but it’s coming. And for older adults? Blood flow restriction training (BFR) is showing promise. It uses a tourniquet to limit blood flow while doing light resistance work. Mayo Clinic’s 2024 study found it cuts recovery time by 30% for patients over 60. No heavy lifting needed.Final Reality Check
Shoulder pain isn’t something you “tough out.” But it’s also not a death sentence for your active life. The vast majority of people recover fully with the right rehab plan. You don’t need surgery. You don’t need endless injections. You need consistency, patience, and the right exercises done at the right time. It’s not glamorous. It’s not quick. But it works.Can shoulder bursitis go away on its own?
Yes, but only if you stop the behaviors that caused it. Rest alone won’t fix it. Without rehab, the inflammation may calm down temporarily, but the underlying muscle imbalances and poor movement patterns stay. That’s why 15-20% of people get the pain back within a year. Active rehab is what prevents recurrence.
How long does rotator cuff rehab take?
Most people see noticeable improvement in 6-8 weeks, but full recovery takes 3-6 months. The first 4 weeks focus on reducing pain and regaining motion. Weeks 5-12 are for rebuilding strength. After that, it’s about maintaining function. Rushing it leads to setbacks.
Is heat or ice better for shoulder bursitis?
Ice is best in the first 3-5 days to reduce swelling and inflammation. After that, heat can help loosen stiffness before exercises. But never use heat if the area is still swollen or hot to the touch-that can make inflammation worse.
Can I still work out with shoulder bursitis?
Yes-but not the way you’re used to. Avoid overhead presses, bench presses, and pull-ups. Stick to lower body workouts, walking, and light cardio. Once you’re past the acute phase, you can start modified shoulder exercises with bands or light dumbbells. Always prioritize form over weight.
What’s the best sleeping position for shoulder pain?
Sleep on your back with a pillow under the painful arm to keep it slightly elevated. If you must sleep on your side, put a pillow between your arms to prevent your shoulder from rolling inward. Avoid sleeping on the affected shoulder-it compresses the inflamed bursa and makes pain worse.
Do I need an MRI for shoulder pain?
Not unless you’ve tried 3-6 months of rehab with no improvement, or if you’ve had a sudden trauma like a fall or dislocation. Most shoulder pain is caused by inflammation and muscle weakness-not tears. MRIs often show “abnormalities” in people with no pain, so they can lead to unnecessary worry or treatment.
Can physical therapy make shoulder pain worse?
Only if it’s done incorrectly. Pushing too hard too soon, using too much resistance, or skipping scapular control exercises can irritate the area. But when guided by a skilled therapist who follows evidence-based protocols, PT reduces pain in 87% of cases, according to patient reviews on Healthgrades.
rasna saha
January 24, 2026 AT 20:31I’ve been dealing with this for 8 months and your post literally made me cry-thank you. I thought I was broken, but now I realize I just needed someone to tell me it’s okay to go slow. Started pendulum exercises yesterday and my shoulder didn’t scream at me. Small wins, right?
James Nicoll
January 25, 2026 AT 02:40So let me get this straight-we’re telling people to do physical therapy instead of surgery… and the real secret is… *consistency*? Shocking. Next you’ll tell me drinking water helps with dehydration. Also, why is everyone suddenly into scapular retraction like it’s the new yoga pose? I’m just here for the memes and the 3am shoulder pain.
Ashley Porter
January 26, 2026 AT 22:55From a biomechanics standpoint, the subacromial space narrowing during the painful arc is a classic impingement cascade-especially when scapular dyskinesis is present. The bursa isn’t just inflamed, it’s being mechanically compressed by aberrant kinematics. Most PTs miss this because they’re focused on rotator cuff activation without addressing proximal control. The 30% faster recovery with scapular work? Totally validates the proximal-to-distal model. Also, PRP is overhyped because the RCTs have low power and high heterogeneity. BFR though? That’s legit for older cohorts-low-load, high-metabolic stress, minimal joint reaction forces. Game changer.
Peter Sharplin
January 28, 2026 AT 09:07Just wanted to add something real quick-don’t ignore the thoracic spine. I’ve seen so many patients with shoulder pain whose real issue is a stiff mid-back. If your thoracic extension is limited, your scapula can’t glide properly. That means even perfect rotator cuff exercises won’t help if your ribcage is locked up. A simple foam roller session on your upper back before your rehab routine? Huge difference. And yes, ice first, then heat. Don’t heat when it’s swollen. I’ve seen too many people turn acute bursitis into chronic bursitis by using heat too early. You’re not a sauna.
shivam utkresth
January 29, 2026 AT 05:09Bro, this is the kind of post that makes me feel like the universe finally sent me a manual for my busted shoulder. I’m from Delhi, and here, everyone just pops painkillers and waits for magic. No one talks about rehab like this. I started the pendulum thing yesterday-felt like a baby learning to walk. But hey, no screaming. Also, the part about weekend warriors? 100% me. Played cricket last Saturday, now I’m back to square one. Lesson learned. No more ‘I’m fine’ lies. Also, scapular retraction? That’s my new mantra. Squeeze like you’re trying to crack a walnut between your shoulder blades. It’s weird. It’s dumb. But it works.
John Wippler
January 30, 2026 AT 12:58Let me tell you something about pain and patience. You don’t heal by pushing through. You heal by showing up-even on the days you feel like a broken toaster. I did this rehab for 14 weeks. Some days I cried. Some days I did one rep. Some days I just sat there breathing and didn’t move at all. And guess what? It worked. Not because I was strong. Because I was stubborn. Not because I followed every rule. Because I listened to my body when it whispered. And now? I can reach for my coffee mug without wincing. That’s not magic. That’s medicine. Real medicine. The kind you have to earn.
Kipper Pickens
January 31, 2026 AT 09:18Medicare’s new reimbursement structure is a textbook example of value-based care shifting incentives toward early PT. The 4.7% bump for supervised therapy? That’s not charity-it’s economics. Less injections means fewer complications, lower downstream costs. The wearable sensor tech is still in beta, but the feedback loop it creates? That’s the future. Real-time kinematic correction beats post-hoc video analysis any day. And BFR? It’s essentially low-load hypertrophy via metabolic stress without mechanical overload. Perfect for older adults with sarcopenia. Just don’t use a tourniquet from a gym band. Use a proper pneumatic cuff. Or you’ll end up with a hematoma and a lawsuit.
Aurelie L.
January 31, 2026 AT 09:47I tried this. It didn’t work. Now I’m on disability. Good luck.