Sodium & Medication Effectiveness Calculator
How Your Sodium Intake Affects Medication
This calculator estimates how your current sodium consumption impacts blood pressure medication effectiveness based on research from the JAMA study. The average American consumes 4,500 mg of sodium daily.
Note: This is for informational purposes only. Never stop or adjust medication without consulting your doctor.
Your Estimated Impact
Personalized Recommendation
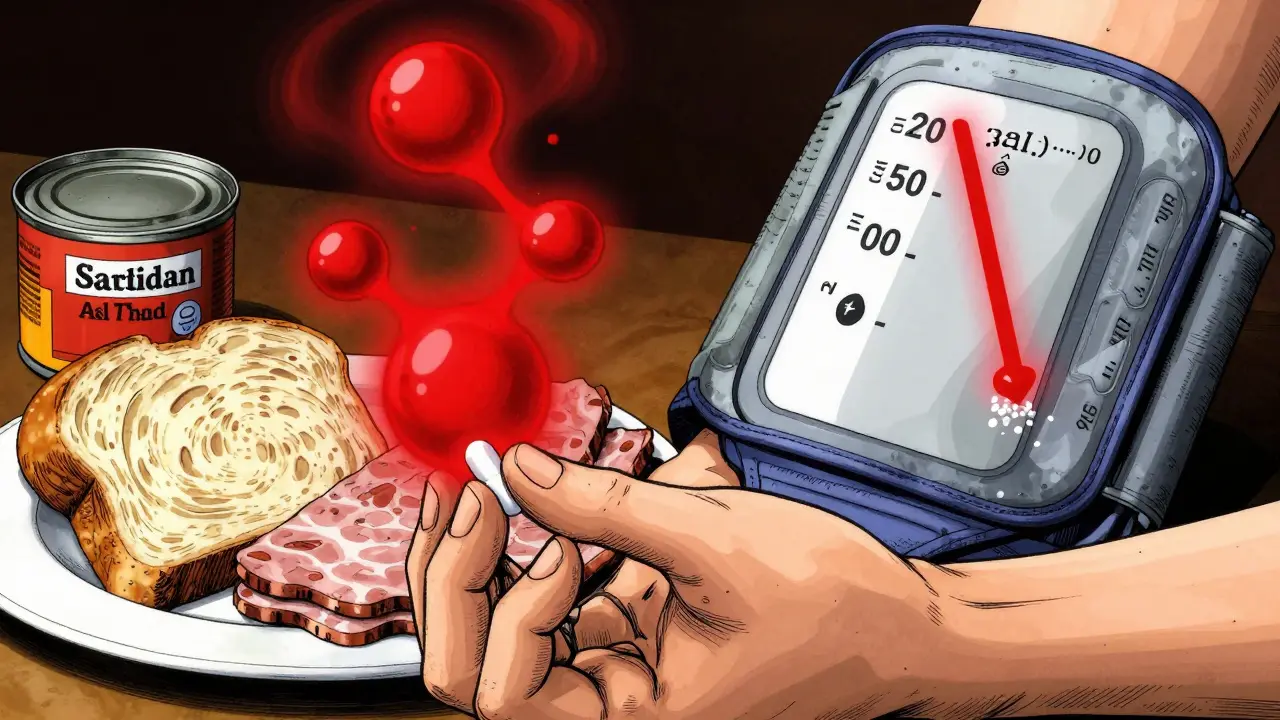
When you take blood pressure medication, you might think the pills are doing all the work. But what you eat - especially how much salt - can make those pills work better… or almost useless. A major 2023 study published in JAMA found that cutting back on salt can lower systolic blood pressure by 6 mm Hg - the same drop you’d get from starting a first-line blood pressure drug. And this isn’t just for people not on meds. Even if you’re already taking ACE inhibitors, diuretics, or ARBs, too much salt is quietly sabotaging their effect.
Why Salt Makes Your Medication Less Effective
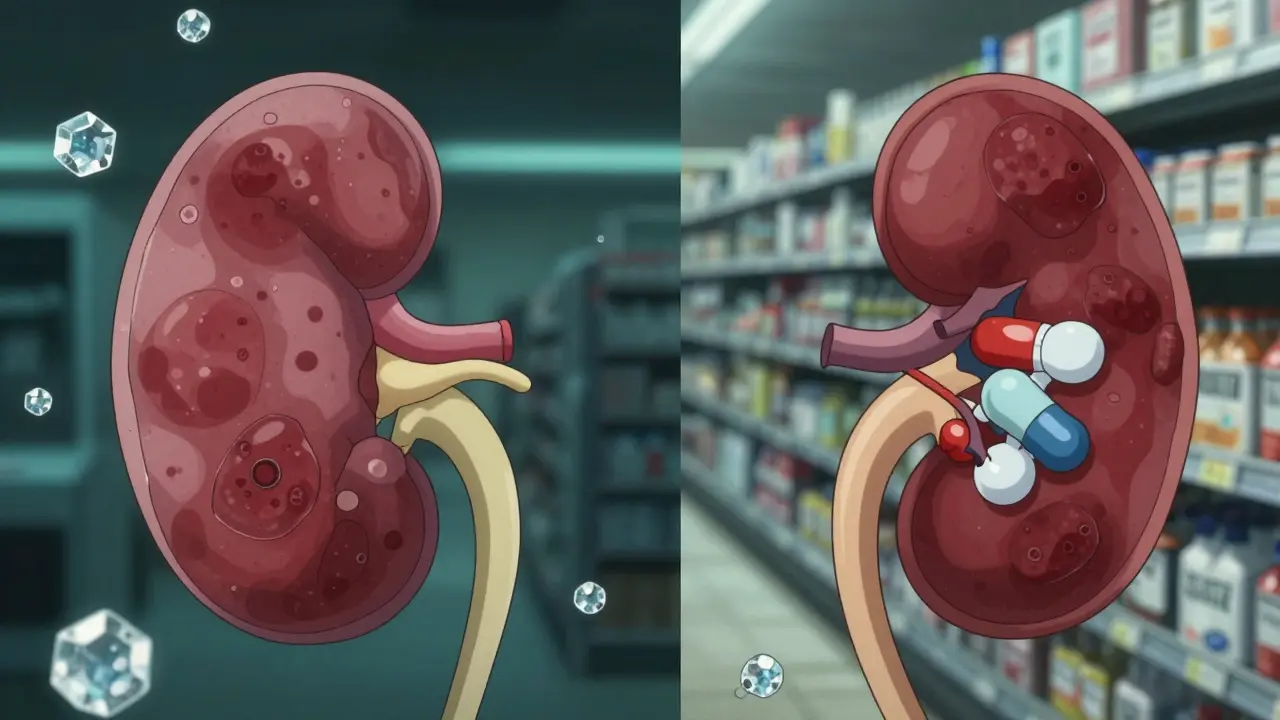
Your body holds onto water when you eat too much sodium. That extra fluid increases pressure on your blood vessel walls, which is exactly what blood pressure meds are trying to fix. When you’re consuming 4,500 mg of sodium a day - the average for most Americans - your body is fighting a constant battle. Medications like diuretics work by flushing out fluid, but if you keep dumping salt into your system, your kidneys just hold onto more water again. ACE inhibitors and ARBs relax blood vessels, but high sodium stiffens them. The result? Your meds are working half as hard.
Research shows that for every 50 mmol drop in daily sodium excretion (roughly 1,150 mg), systolic blood pressure falls by about 1.1 mm Hg. For people with high blood pressure, that effect is even stronger - up to twice as much. One study found that 73.4% of participants saw a meaningful drop in pressure just by lowering sodium. Nearly half of them were labeled “salt sensitive,” meaning their blood pressure dropped 5 mm Hg or more.
How Much Salt Are You Really Eating?
Most people think they’re cutting salt by skipping the salt shaker. But that’s not where the problem is. About 70% of the sodium we eat comes from packaged foods and restaurants - things like bread, canned soup, deli meats, frozen meals, and even breakfast cereal. A single slice of commercial bread can have 230 mg of sodium. A small container of yogurt? 120 mg. A typical sandwich from a deli? Easily over 1,500 mg before you even add chips or pickles.
The American Heart Association recommends no more than 2,300 mg daily - and ideally 1,500 mg for people with hypertension. But the average American eats 3,400 mg. In the JAMA study, participants averaged 4,500 mg. That’s nearly double the limit.
What Happens When You Cut Salt - Fast
You don’t need to wait months to see results. In the same 2023 study, participants switched from their usual high-sodium diet to one with only 500 mg of sodium per day. Within just seven days, their systolic blood pressure dropped an average of 7-8 mm Hg. That’s faster than waiting for a new prescription to kick in.
Even small changes matter. Switching from a 2,200 mg added-sodium diet to 500 mg total dropped pressure by 7-8 mm Hg. Going from your normal diet (4,500 mg) to 2,300 mg still gave a 6 mm Hg drop - the same as starting a pill. And the benefits aren’t just about numbers. Lower sodium also reduces protein in urine, which means less strain on your kidneys. That’s especially important if you have diabetes or kidney disease, where meds like ACE inhibitors are used to protect kidney function - but only if salt isn’t undoing their work.
Which Medications Benefit Most?
Not all blood pressure drugs respond the same way to sodium reduction. Diuretics - like hydrochlorothiazide - are designed to get rid of fluid. But if you keep eating salty food, your body just reabsorbs it. Reducing sodium makes diuretics work better and may even let your doctor lower your dose.
ACE inhibitors (lisinopril, enalapril) and ARBs (losartan, valsartan) rely on relaxing blood vessels. High sodium makes those vessels stiff and resistant. Cutting salt helps them do their job. Beta-blockers and calcium channel blockers also respond better, though less dramatically.
One key insight: if your blood pressure isn’t improving despite taking meds, high sodium intake might be the hidden reason. Doctors often assume the medication isn’t working - but sometimes, it’s your diet.
How to Actually Reduce Sodium - Without Giving Up Flavor
You don’t need to eat bland food. Here’s how to cut sodium without sacrificing taste:
- Read labels - Look for “mg of sodium,” not % Daily Value. Choose products with under 140 mg per serving.
- Avoid processed meats - Deli turkey, bacon, sausage, and hot dogs are sodium bombs. Swap for fresh, unprocessed chicken or fish.
- Cook at home - Use herbs, garlic, lemon, vinegar, and spices instead of salt. Cumin, paprika, oregano, and black pepper add big flavor with zero sodium.
- Choose low-sodium versions - Many brands now offer “no salt added” soups, beans, and sauces. They taste fine - and they make a difference.
- Watch out for hidden salt - Tomato sauce, salad dressings, soy sauce, and condiments can pack 400-600 mg per tablespoon. Try reducing or switching to low-sodium options.
- Be careful with salt substitutes - Potassium chloride can help, but if you have kidney disease or take certain meds (like ACE inhibitors), too much potassium can be dangerous. Always check with your doctor first.
Who Doesn’t Benefit?
Not everyone responds the same. About 25-30% of people are “salt resistant” - their blood pressure barely budges when they cut salt. But that doesn’t mean salt doesn’t affect them. Even in these cases, high sodium still increases stress on the heart, kidneys, and blood vessels. So while their numbers might not change much, long-term damage risk does.
Older adults, Black individuals, and those with higher baseline blood pressure tend to see the biggest drops. But that doesn’t mean younger or lighter individuals shouldn’t cut back. The science is clear: reducing sodium helps everyone - even if the effect isn’t dramatic on the scale.
What’s Changing in 2026?
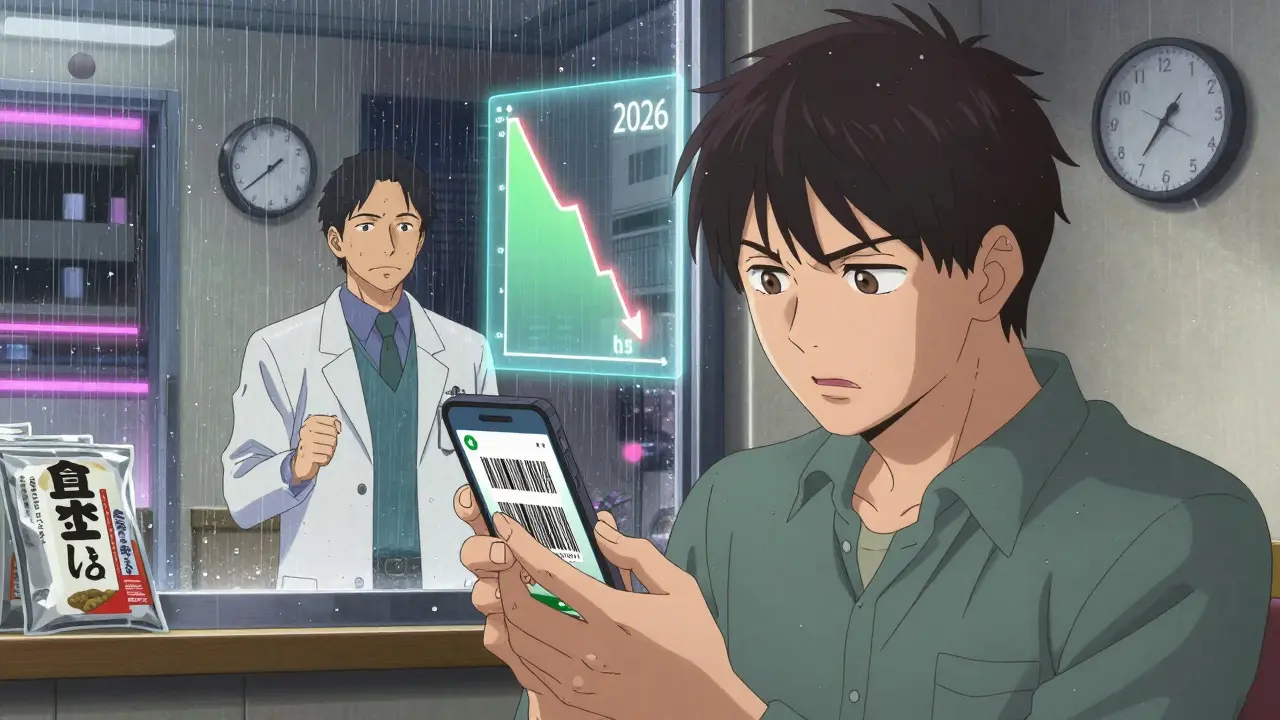
The FDA’s 2023 voluntary sodium reduction targets for food manufacturers are starting to take effect. By 2026, average sodium intake in the U.S. is projected to drop to 3,000 mg daily - still too high, but a step forward. Some companies are reformulating products. You’ll see more “low sodium” labels on packaged foods.
Meanwhile, researchers are testing mobile apps that track sodium intake and alert users when their salt consumption might interfere with their meds. One app, currently in Phase II trials, lets users scan barcodes and instantly see how their sodium intake affects their blood pressure medication. It’s not available yet - but it’s coming.
What You Should Do Today
If you’re on blood pressure medication:
- Check your daily sodium intake. Use a free app like MyFitnessPal for a week - you’ll be surprised.
- Swap one high-sodium item per day. Replace canned soup with homemade broth. Swap deli meat for grilled chicken.
- Don’t add salt at the table. Taste your food first. You might not need it.
- Ask your doctor if your meds could be adjusted. Lower sodium might mean lower doses.
- Give it three weeks. You’ll likely feel less bloated, sleep better, and notice your blood pressure improving.
This isn’t about perfection. It’s about progress. Even cutting 1,000 mg of sodium a day can help your meds work better. And that’s a win - no new prescription needed.
Can I stop my blood pressure medication if I cut salt?
No. Never stop or change your medication without talking to your doctor. While cutting salt can improve how well your meds work - and may even allow your doctor to lower your dose - it doesn’t replace them. Blood pressure medication prevents long-term damage to your heart, kidneys, and brain. Sodium reduction supports that, but doesn’t substitute for it.
How long does it take to see a difference after cutting salt?
Many people notice changes within a week. In the 2023 JAMA study, systolic blood pressure dropped by 6-8 mm Hg in just seven days after switching to a low-sodium diet. Some feel less bloated or notice better sleep sooner. Consistent low sodium over weeks leads to more stable, lasting results.
Is sea salt or Himalayan salt better than table salt?
No. All salt - whether table, sea, or Himalayan - is mostly sodium chloride. The trace minerals in colored salts are too small to make a health difference. A teaspoon of any salt contains about 2,300 mg of sodium. If you’re trying to cut sodium, switching salt types won’t help. Focus on reducing total amount, not type.
Can I use salt substitutes?
Potassium chloride salt substitutes can help reduce sodium, but they’re not safe for everyone. If you have kidney disease, take ACE inhibitors, ARBs, or certain diuretics, too much potassium can build up in your blood and cause dangerous heart rhythms. Always check with your doctor before using a salt substitute.
Do I need to eliminate salt completely?
No. Your body needs a small amount of sodium - about 500 mg per day - to function. The goal isn’t zero salt. It’s getting from 4,500 mg down to under 2,300 mg, and ideally under 1,500 mg if you have high blood pressure. That’s still plenty of room to enjoy flavorful food - you just need to choose it wisely.
Coy Huffman
February 4, 2026 AT 07:13Amit Jain
February 5, 2026 AT 09:19Alec Stewart Stewart
February 5, 2026 AT 15:45Demetria Morris
February 6, 2026 AT 11:43Geri Rogers
February 8, 2026 AT 04:09Samuel Bradway
February 9, 2026 AT 01:36caroline hernandez
February 9, 2026 AT 20:55Jhoantan Moreira
February 11, 2026 AT 02:33