What Is Retinal Vein Occlusion?
Retinal vein occlusion (RVO) happens when a vein in the retina gets blocked, stopping blood from flowing out. This causes fluid and blood to leak into the retina, leading to swelling-especially in the macula, the part of the eye responsible for sharp central vision. The result? Sudden, painless blurring or loss of vision in one eye. It doesn’t hurt, which is why many people don’t realize something’s wrong until their vision is already affected.
There are two main types: central retinal vein occlusion (CRVO), which blocks the main vein, and branch retinal vein occlusion (BRVO), which affects smaller branches. BRVO is more common and often happens where a hardened artery crosses over a vein and squeezes it shut. CRVO tends to cause more severe vision loss.
It’s not rare. Around 16.4 million people worldwide have RVO, and it’s one of the top causes of vision loss after diabetic eye disease and glaucoma. Most cases happen after age 55, but it can strike younger people too-especially those with blood disorders or who take birth control pills.
Who’s Most at Risk?
If you’re over 65, you’re at higher risk. About half of all RVO cases happen in people over that age. But age isn’t the only factor. The biggest medical risk is high blood pressure. Up to 73% of CRVO patients over 50 have it. Even if you think your blood pressure is under control, unmanaged hypertension is the number one driver of vein blockages in the eye.
Diabetes is another major player. About 10% of RVO patients over 50 have diabetes, and those who do tend to have worse vision outcomes. High cholesterol also plays a role-35% of people with RVO have total cholesterol above 6.5 mmol/L. It’s not just about eating too much fat; it’s about plaque building up in arteries, which then press on nearby veins.
Glaucoma raises the risk too, especially when pressure inside the eye pushes on the optic nerve where the retinal vein exits. If you have glaucoma and suddenly notice blurry vision, get your eyes checked right away.
Lifestyle matters. Smoking increases your risk by 25-30%. Being overweight or inactive adds to the problem. Hardened arteries don’t just affect your heart-they clog your eyes too.
For younger patients under 45, the story changes. About 5-10% of RVO cases happen in this group. In women, birth control pills are the most common link to CRVO. Blood disorders like polycythemia vera, leukemia, or inherited clotting conditions like factor V Leiden can also trigger it. If you’re young and get RVO, your doctor will likely run blood tests to rule these out.
How Are RVO Injections Used to Treat Vision Loss?
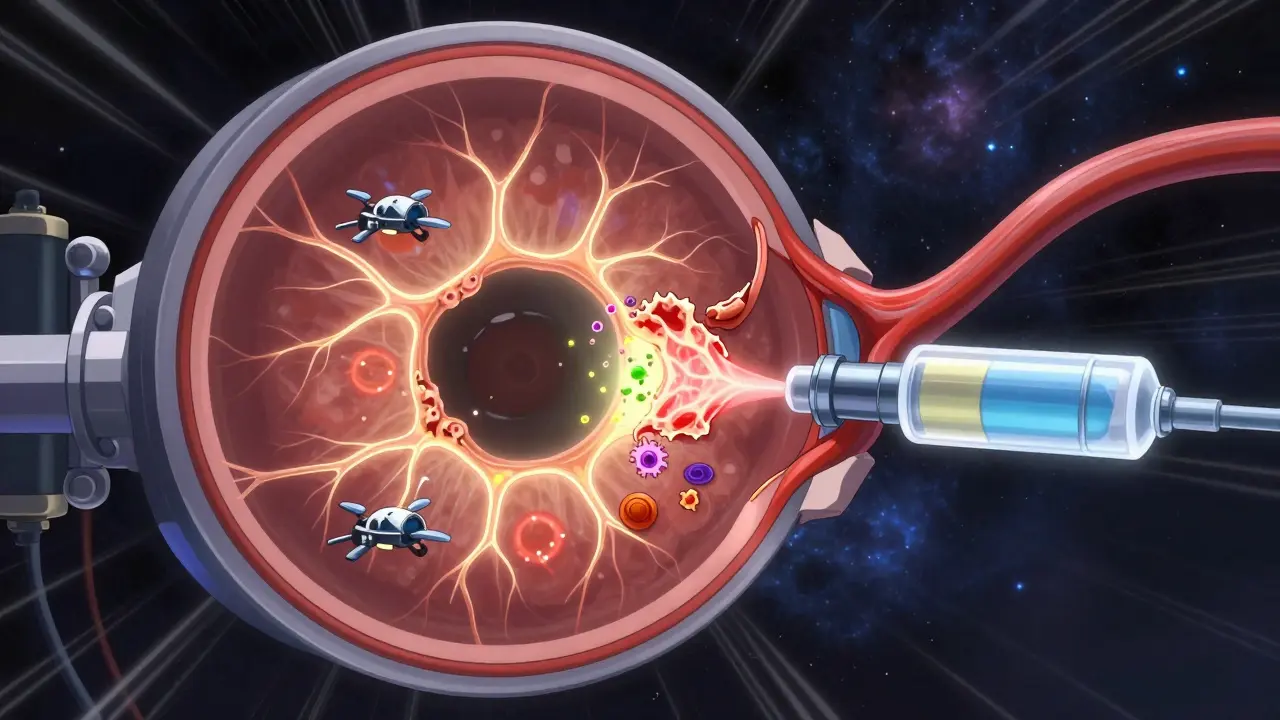
There’s no way to unblock the vein once it’s clogged. Treatment doesn’t fix the blockage-it tackles the damage it causes. The biggest problem is macular edema, when fluid builds up in the macula and blurs your vision. That’s where injections come in.
The two main types of injections are anti-VEGF drugs and corticosteroids. Anti-VEGF drugs like ranibizumab (Lucentis), aflibercept (Eylea), and bevacizumab (Avastin) block a protein called VEGF that causes leaky blood vessels. By stopping this protein, they reduce swelling and help vision improve.
Studies show these drugs work. In the BRAVO trial, people using ranibizumab gained an average of 16.6 letters on the eye chart after a year. That’s from reading 20/200 to 20/60-enough to drive again or read a phone screen clearly. Aflibercept showed similar results in the COPERNICUS trial.
Corticosteroid injections, like the dexamethasone implant (Ozurdex), are a second option. They reduce inflammation and swelling too, but they come with trade-offs. About 60-70% of people who get this implant develop cataracts within a year. One in three get higher eye pressure, which can lead to glaucoma. That’s why doctors usually try anti-VEGF first.
How Often Do You Need Injections?
It’s not a one-and-done deal. Most people start with monthly injections until the swelling goes down. Then, they switch to as-needed shots based on eye scans.
Doctors use optical coherence tomography (OCT) to measure fluid in the macula. Treatment usually starts when the central subfield thickness is over 300 micrometers. Once it drops below 250, they pause treatment and monitor.
Real-world data shows patients need 8-12 injections in the first year. Some need more. The American Academy of Ophthalmology recommends continuing treatment as long as fluid returns. Stopping too soon means vision can drop again.
Newer protocols like treat-and-extend are changing the game. Instead of monthly shots, you get one every four weeks, then stretch it to six, then eight, then 12-if your eye stays dry. The COMINO study found this approach gives the same results with 30% fewer injections.
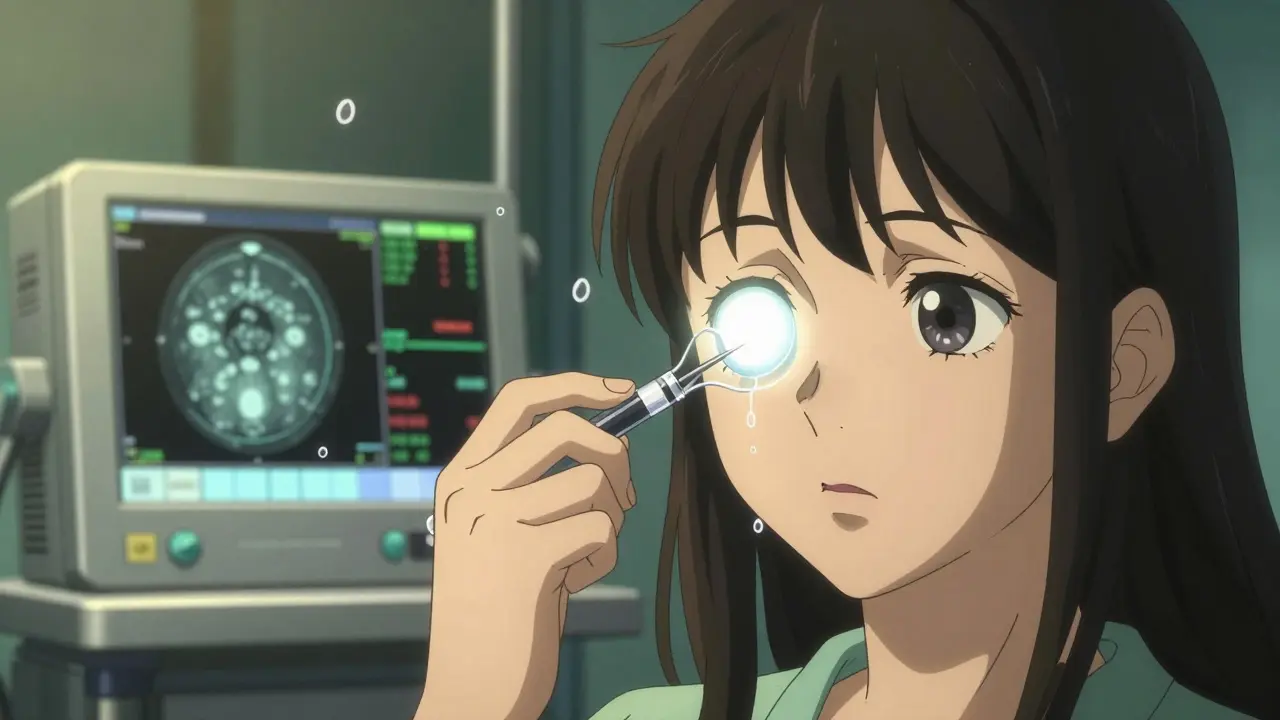
What’s It Like to Get an Eye Injection?
It sounds scary. It’s not. The procedure takes 5-7 minutes. Your eye is numbed with drops. The doctor cleans the surface with iodine. A tiny speculum holds your eyelid open. Then, with a very fine needle, they inject the medicine into the white part of your eye, just behind the iris.
You might feel pressure. Some people feel a quick pinch. Most say it’s less painful than a mosquito bite.
Side effects are common but usually mild. About 25-30% get a red spot on the white of the eye from a small bleed. About 15-20% feel a spike in eye pressure right after, which goes down in hours. Floaters are normal too-they clear up in a few days.
Serious problems like infection (endophthalmitis) happen in less than 1 in 1,000 injections. That’s rarer than being struck by lightning.
But the real challenge isn’t the shot-it’s the mental toll. Many patients describe anxiety before each visit. One person on Reddit said, “My heart races even though I know it’s routine.” Others feel exhausted from the schedule. After 18 months of monthly visits, some stop going because the stress outweighs the benefit.
Cost and Access to Treatment
Cost is a huge barrier. In the U.S., a single dose of Lucentis or Eylea costs about $2,000. Avastin, which is used off-label, costs around $50. That’s why safety-net clinics use Avastin for 60-70% of RVO cases, while private practices use the brand-name drugs more often.
Insurance helps, but copays still hurt. One patient shared on a forum that $150 per injection added up fast on a fixed income. Ozurdex implants cost $2,500 out-of-pocket-more than a year’s worth of Avastin.
Some patients get better results with cheaper options. One person reported no improvement after eight Avastin shots, but gained 10 lines of vision after one Ozurdex implant. Others see the opposite. That’s why treatment isn’t one-size-fits-all.
What’s Next for RVO Treatment?
The future is about reducing burden. New drugs like OPT-302 are being tested in combination with aflibercept to target more types of VEGF. If it works, it could help patients who don’t respond to current treatments.
Gene therapy is also on the horizon. RGX-314, currently in trials, aims to give your eye the ability to make its own anti-VEGF protein-potentially eliminating the need for injections altogether. Early results show promise.
Then there’s the Port Delivery System (Susvimo), a tiny refillable implant already approved for macular degeneration. It’s being tested for RVO. If approved, it could mean just two refills a year instead of 12 injections.
Doctors are also using optical coherence tomography angiography to see blood flow in the retina in real time. This helps predict who will respond to treatment and who needs a different approach.
What Should You Do If You’re Diagnosed?
First, don’t panic. Vision loss from RVO can improve-with treatment. About 78% of patients gain meaningful vision after a year of anti-VEGF therapy.
Second, manage your health. Control your blood pressure. Lower your cholesterol. Quit smoking. If you have diabetes, keep your A1C under 7%. These steps won’t fix your eye, but they’ll prevent it from getting worse-and stop the other eye from being affected.
Third, stick with treatment. Missing appointments is the #1 reason vision doesn’t improve. Even if you feel fine, fluid can build up silently. OCT scans catch it before you notice.
Finally, talk to your doctor about your options. If you’re struggling with cost, ask about Avastin. If you’re tired of shots, ask about Ozurdex or upcoming trials. You’re not just a patient-you’re part of the treatment team.
Can RVO Be Prevented?
Not always. But you can lower your risk. Get regular eye exams after 50-even if you see fine. High blood pressure and cholesterol often have no symptoms until damage is done. A simple eye check can catch early signs of vein stress before a full blockage happens.
If you’re under 45 and have unexplained vision loss, don’t assume it’s just eye strain. Ask about blood tests for clotting disorders. If you’re on birth control and have a family history of clots, talk to your doctor about alternatives.
Living a healthy life-eating well, moving daily, not smoking-is the best defense. RVO isn’t just an eye disease. It’s a warning sign your whole vascular system is under strain.

Celia McTighe
December 28, 2025 AT 11:22Debra Cagwin
December 28, 2025 AT 19:09Kelsey Youmans
December 28, 2025 AT 22:41Ryan Touhill
December 30, 2025 AT 02:35Hakim Bachiri
December 31, 2025 AT 15:24oluwarotimi w alaka
January 1, 2026 AT 17:21ANA MARIE VALENZUELA
January 3, 2026 AT 15:10Teresa Marzo Lostalé
January 5, 2026 AT 03:30Sydney Lee
January 6, 2026 AT 11:11