Pharmacogenomics Medication Interaction Checker
Check how your genes might affect your response to common medications. Based on CPIC (Clinical Pharmacogenetics Implementation Consortium) guidelines.
Pharmacogenomics Results
Note: These results are based on CPIC guidelines. They should be interpreted by a healthcare professional alongside other clinical factors.
Every year, over 100,000 people in the U.S. die from reactions to medications they were prescribed. Many of these deaths aren’t due to mistakes - they’re because the drug simply didn’t match the patient’s biology. That’s where pharmacogenomics testing comes in. It’s not science fiction. It’s not a luxury. It’s a practical tool that uses your DNA to predict how your body will react to drugs - before you even take them.
What Is Pharmacogenomics Testing?
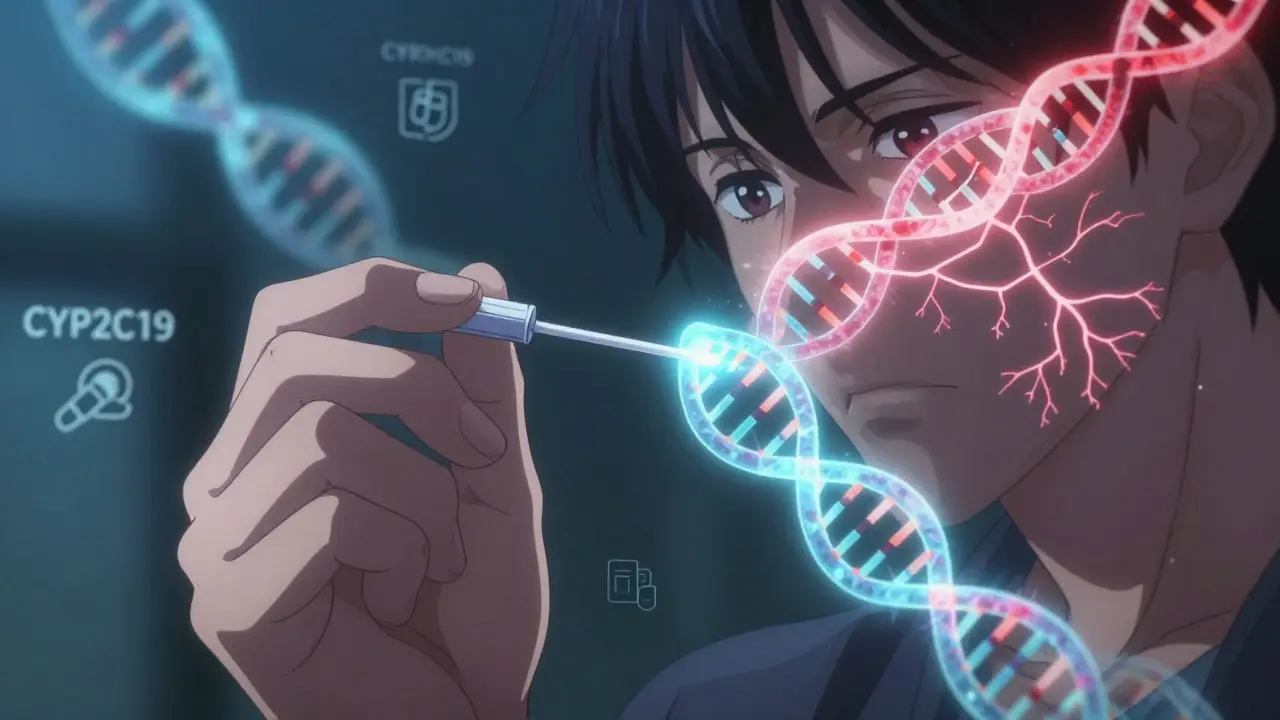
Pharmacogenomics testing looks at specific genes that control how your body breaks down and responds to medications. Think of it like a personalized instruction manual for your drugs. Two people can take the same pill, but one might feel great while the other gets sick - not because of dosage errors, but because of differences in their genes. The key players here are enzymes like CYP2D6, CYP2C19, and CYP2C9. These are part of the cytochrome P450 family, responsible for processing about 75% of all prescription drugs. If your version of the CYP2D6 gene makes you a slow metabolizer, you might build up toxic levels of certain antidepressants or painkillers. If you’re a fast metabolizer, the drug might leave your system too quickly to work at all. The FDA has identified 178 drugs with pharmacogenomic information in their labels. That includes common ones like clopidogrel (Plavix), warfarin, and abacavir. For abacavir, a simple genetic test for the HLA-B*57:01 variant is required before prescribing - because without it, up to 60% of carriers could suffer a life-threatening allergic reaction.How It Works in Practice
Getting tested is straightforward. A saliva swab or blood sample is sent to a CLIA-certified lab. Results typically come back in 3 to 14 days. Most clinical tests focus on targeted gene panels - not your entire genome. A standard panel might check 10 to 20 genes linked to 50 to 100 drugs, costing between $250 and $500. The results aren’t just a list of variants. They’re interpreted using guidelines from organizations like CPIC (Clinical Pharmacogenetics Implementation Consortium) and DPWG. These groups review hundreds of studies and assign clear recommendations: “Use drug X at lower dose,” “Avoid drug Y,” or “Consider drug Z instead.” One real-world example: a patient with depression tried five antidepressants with no success. A pharmacogenomic test showed they were a CYP2D6 poor metabolizer. Switching from SSRIs (which rely on CYP2D6) to bupropion - which doesn’t - led to symptom relief within weeks. That’s not rare. A 2022 meta-analysis found pharmacogenomic-guided antidepressant treatment led to a 30.5% higher remission rate than standard care.Where It Makes the Biggest Difference
Pharmacogenomics isn’t useful for every drug. It shines where small biological differences have big consequences.- Psychiatry: Up to 60% of patients don’t respond to their first antidepressant. Testing cuts trial-and-error time and reduces side effects.
- Cardiology: About 30% of people have a CYP2C19 variant that makes clopidogrel ineffective. For them, switching to prasugrel or ticagrelor cuts heart attack risk by half.
- Oncology: Tamoxifen for breast cancer requires CYP2D6 to become active. Poor metabolizers get little benefit - testing helps avoid ineffective treatment.
- Pain Management: Codeine and tramadol rely on CYP2D6 to turn into their active forms. Ultra-rapid metabolizers can overdose on morphine-like compounds; poor metabolizers get no pain relief.
What the Evidence Says
The data is growing fast. A 2021 study in Clinical Pharmacology & Therapeutics found pharmacogenomic testing could reduce adverse drug reactions by up to 30%. The American College of Medical Genetics and Genomics now endorses pre-emptive testing for 11 gene-drug pairs with strong evidence - including genes linked to warfarin, clopidogrel, and statins. But it’s not perfect. Genes explain only 10-15% of why people respond differently to most drugs. Other factors - age, liver function, diet, other medications, even gut bacteria - play big roles too. That’s why testing doesn’t replace clinical judgment. It informs it. Some critics point out that most studies come from populations of European descent. Non-European groups are underrepresented in genetic databases, meaning recommendations may not apply equally. That’s changing - the NIH’s All of Us program is sequencing genomes from over 620,000 people, with diverse ancestry, and returning pharmacogenomic results to participants starting in 2023.Barriers to Adoption
Despite the evidence, pharmacogenomics testing is still far from routine. Only 15% of physicians feel confident interpreting results. Many EHR systems don’t automatically flag gene-drug conflicts. And insurance coverage? Patchy at best. Only 35% of commercial plans cover testing, though Medicare Part B does for specific cases like clopidogrel before stent placement. Patients often get confused. One Reddit user wrote: “I paid $400 for a test. My doctor didn’t know what to do with the results.” That’s common. The real bottleneck isn’t the science - it’s the system. Providers need training. Labs need to deliver clear, actionable reports. Pharmacies need to integrate alerts into their dispensing systems. Some health systems are solving this. The University of Florida automated clinical decision support into their EHR. When a doctor prescribes a drug that conflicts with a patient’s known gene variant, the system pops up a warning - with a suggested alternative. Time to act dropped from two weeks to under 48 hours.
Who Offers Testing?
Several companies specialize in clinical pharmacogenomics:- OneOme: Offers RightMed, FDA-cleared for 24 genes and over 350 medications. Known for strong clinical support and integration tools.
- Invitae: Acquired Good Start Genetics in 2019. Offers broad panels and works with major insurers.
- Quest Diagnostics: Launched PGxRight in 2020. Integrates with hospital labs and EHRs.
What’s Next?
The future is moving fast. In 2023, the FDA approved the first next-generation sequencing test for pharmacogenomics. Researchers are developing polygenic risk scores - combining dozens of genes to predict drug response more accurately. Point-of-care devices that give results in under an hour are in clinical trials. By 2027, experts predict 30% of prescriptions will include pharmacogenomic data - up from less than 5% today. By 2030, half of all U.S. adults could have their pharmacogenomic profile stored in their medical record. The potential savings are huge. The Rand Corporation estimates widespread use could save the U.S. healthcare system $137 billion a year by avoiding hospitalizations from bad drug reactions and prescribing more effective treatments from day one.Should You Get Tested?
If you’ve had multiple medications fail, or experienced serious side effects, it’s worth asking your doctor. It’s especially helpful if you’re on:- Antidepressants or antipsychotics
- Heart medications like clopidogrel or warfarin
- Opioids or codeine for pain
- Chemotherapy drugs like tamoxifen or 5-FU
Is pharmacogenomics testing covered by insurance?
It depends. Medicare Part B covers testing for specific drugs like clopidogrel before stent placement. Most private insurers cover it only if there’s a clear medical reason - like multiple failed antidepressants or a history of severe side effects. About 35% of commercial plans offer coverage. Always check with your insurer and ask for pre-authorization.
How accurate are pharmacogenomic test results?
The genetic variants tested are highly accurate - labs use FDA-cleared methods with over 99% precision. But the interpretation is where context matters. A variant might mean you’re a slow metabolizer, but your liver health, age, or other drugs you take can change how that plays out. Results are guidelines, not absolutes.
Can pharmacogenomics testing help with over-the-counter drugs?
Not usually. Most OTC drugs like ibuprofen or acetaminophen have wide safety margins and aren’t strongly affected by common genetic variants. Testing focuses on prescription drugs where small differences in metabolism can lead to serious harm or lack of effectiveness.
Does pharmacogenomics testing replace therapeutic drug monitoring (TDM)?
No. They’re complementary. TDM measures actual drug levels in your blood - useful for drugs like lithium or vancomycin where levels must stay in a narrow range. Pharmacogenomics predicts how you’ll metabolize a drug before you take it. Some patients benefit from both: genetic info to choose the right drug, then TDM to fine-tune the dose.
How long do pharmacogenomic test results last?
Forever. Your genes don’t change. Once you’ve been tested, the results apply for life. That’s why many experts recommend pre-emptive testing - getting it done once and storing the results in your medical record so future doctors can use them.
Can pharmacogenomics testing reveal other health risks?
Clinical pharmacogenomic tests are designed to look only at genes related to drug metabolism. They don’t screen for disease risks like BRCA mutations or Alzheimer’s. However, some comprehensive panels may include incidental findings. Always ask the lab what genes they’re analyzing and whether you’ll receive results beyond drug response.
Is pharmacogenomics testing only for adults?
No. Children can benefit too, especially in psychiatry, oncology, and epilepsy. For example, testing for CYP2D6 before giving codeine to a child is now recommended - because some kids metabolize it too quickly and can overdose. Pediatric pharmacogenomics is growing fast, especially in academic hospitals.
Susie Deer
January 16, 2026 AT 06:43Andrew Freeman
January 18, 2026 AT 01:40Allison Deming
January 18, 2026 AT 08:24Sarah Triphahn
January 19, 2026 AT 18:30says haze
January 21, 2026 AT 15:58Alvin Bregman
January 23, 2026 AT 12:52Henry Sy
January 23, 2026 AT 19:17Vicky Zhang
January 25, 2026 AT 07:56Jason Yan
January 25, 2026 AT 19:53Sarah -Jane Vincent
January 26, 2026 AT 05:33shiv singh
January 27, 2026 AT 00:20Dylan Livingston
January 27, 2026 AT 08:40Anna Hunger
January 28, 2026 AT 10:47