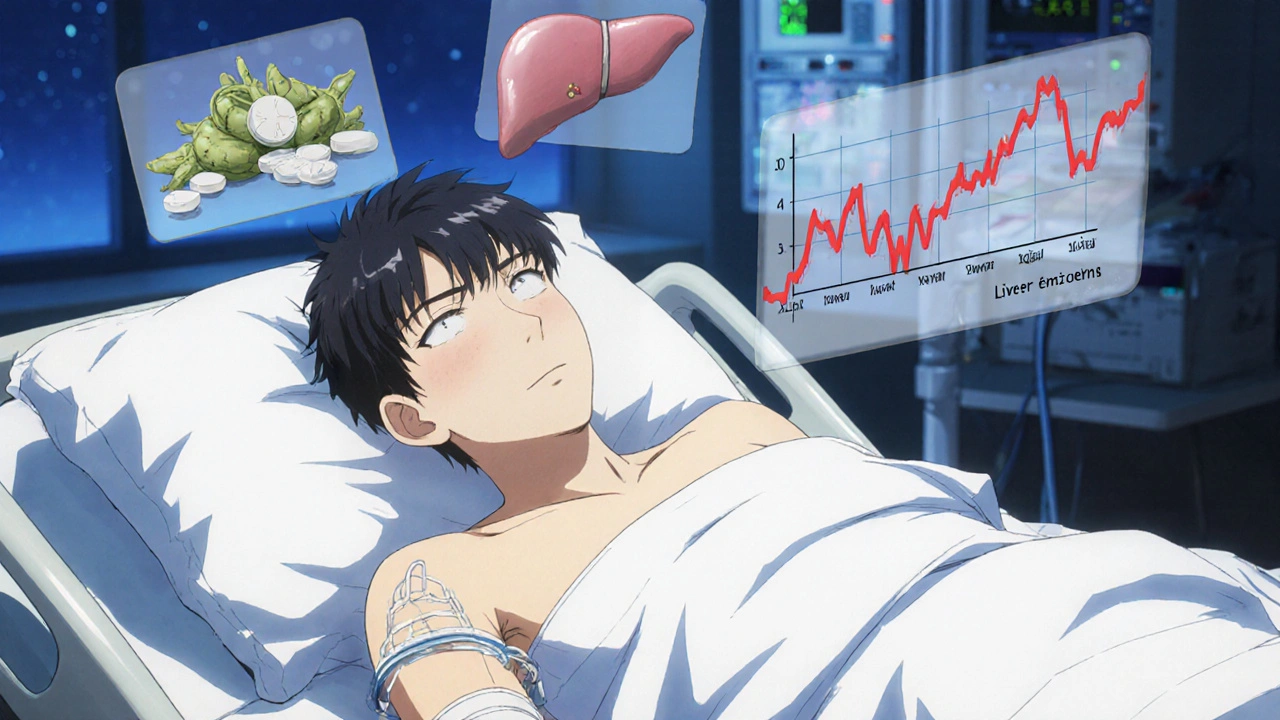
If you're taking medication for anxiety, sleep, or pain-and you're also using kava-you need to hear this. Kava, a plant-based supplement often marketed as a natural remedy for stress, can dangerously boost the effects of sedatives like benzodiazepines, sleep pills, and even alcohol. Worse, it can quietly damage your liver without warning. This isn’t theory. It’s documented in hospitals, FDA reports, and real patient cases.
What Kava Actually Does to Your Body
Kava comes from the roots of Piper methysticum, a plant used for centuries in Pacific Island ceremonies. Today, it’s sold in capsules, teas, and tinctures as an anxiety reliever. Its active compounds, called kavalactones, work on the brain’s GABA receptors-same as Xanax, Valium, and other prescription sedatives. That’s why people feel calm, relaxed, even slightly drowsy after taking it.
But here’s the catch: kava doesn’t just affect your brain. It also interferes with your liver’s ability to process medications. The liver uses enzymes-mainly CYP2D6, CYP2C9, and CYP3A4-to break down drugs. Kavalactones block these enzymes. When you take kava with a sedative, your body can’t clear the medication fast enough. The result? Higher drug levels in your blood, longer sedation, and a higher risk of overdose.
One 2023 Sacramento County case study showed a 42-year-old man taking 300 mg of kava daily with 2 mg of alprazolam (Xanax). Within three months, his liver enzymes spiked to 2,840 U/L (normal is under 40). He developed jaundice and needed hospitalization. That’s not rare. The FDA has logged 37 reports of excessive sedation from kava combined with prescription drugs since 2019. Twelve of those cases required emergency care.
Why Kava Is Riskier Than Other Herbal Supplements
People often assume herbal = safe. But kava is different from valerian, chamomile, or passionflower. Those herbs have minimal drug interactions. Kava? It’s a known major interaction risk with CNS depressants.
Compared to prescription anxiolytics like buspirone or SSRIs, kava lacks standardization. A capsule labeled “250 mg kava” might contain anywhere from 150 to 300 mg of kavalactones depending on how it was extracted. Alcohol-based extracts-common in store-bought supplements-concentrate the toxins more than traditional water-based brews. That’s why the World Health Organization found traditional kava drinks have 9 times fewer adverse events than commercial extracts.
And unlike prescription drugs, kava isn’t monitored. No batch testing. No consistent dosing. No mandatory safety labels. You could buy two bottles from the same brand and get completely different potency. That’s why a Reddit user in 2023 reported being unable to stand for eight hours after mixing kava with 0.5 mg of lorazepam. That’s not a bad reaction-it’s a predictable one.
How Kava and Sedatives Together Can Overwhelm Your Liver
Liver damage from kava doesn’t come with a warning sign. No rash. No fever. Just fatigue, nausea, dark urine, and yellowing skin-symptoms that often appear months after starting use. By then, it might be too late.
Over 25 international cases have been linked to kava-induced liver failure. Some required transplants. The FDA issued a warning in 2002 and has maintained it ever since. Countries like the UK, Canada, and Switzerland banned kava entirely. The EU calls its risk-benefit profile “unfavorable.” Australia says the risk is low-but only if you avoid high doses and don’t mix it with meds.
Here’s the hard truth: if you’re already on sedatives, your liver is under extra strain. Adding kava is like pouring gasoline on a small fire. The combination doesn’t just increase sedation-it can trigger acute hepatitis, cirrhosis, or liver necrosis. A 2024 California Department of Public Health report confirmed kava inhibits the same enzymes that metabolize 80% of commonly prescribed drugs, including antidepressants, painkillers, and antipsychotics.
Who Should Never Use Kava
There are clear groups who should avoid kava completely:
- Anyone taking benzodiazepines (alprazolam, lorazepam, diazepam)
- Anyone on sleep aids (zolpidem, eszopiclone)
- Anyone using opioids, muscle relaxants, or antihistamines with sedative effects
- People with pre-existing liver disease (hepatitis, fatty liver, cirrhosis)
- Those who drink alcohol regularly
- Anyone over 65 or with low body weight
Even if you don’t have liver disease now, kava can trigger damage in otherwise healthy people. The National Institutes of Health says the mechanism isn’t fully understood, but it likely involves genetic susceptibility and long-term enzyme suppression. You might be fine for months-then suddenly, your liver fails.
What to Do If You’re Already Using Kava with Medications
If you’re currently taking kava and a sedative, don’t stop abruptly. Talk to your doctor. Here’s what to do:
- Stop kava immediately if you feel unusually tired, nauseous, or notice yellowing in your eyes or skin.
- Ask your doctor for a liver function test (ALT, AST, bilirubin). Normal levels don’t guarantee safety, but spikes above 3 times the upper limit mean you need to stop kava right away.
- Report your kava use to every healthcare provider-even your dentist. Only 22% of patients mention kava when asked about supplements, according to Sacramento County research.
- Don’t assume “natural” means safe. Kava isn’t regulated like medicine. It’s sold as a supplement, meaning no proof of safety is required before sale.
Most mild liver injuries from kava resolve within 60 days of stopping use. But severe cases? They can be fatal. The American Association for the Study of Liver Diseases recommends discontinuing kava at the first sign of elevated liver enzymes. Don’t wait for symptoms.

Alternatives to Kava for Anxiety and Sleep
You don’t need kava to manage anxiety or improve sleep. Safer, proven options exist:
- Cognitive Behavioral Therapy (CBT): Proven to reduce anxiety as effectively as medication-with no side effects.
- Melatonin (3-5 mg): For sleep onset. No liver risk. No drug interactions.
- Valerian root: Mild sedative. Minimal interaction risk. Less potent than kava, but safer.
- Prescription alternatives: Buspirone, hydroxyzine, or low-dose SSRIs under medical supervision.
And if you’re drawn to kava for its calming effect, consider traditional water-based preparations from reputable sources. Studies show these contain fewer toxic compounds than alcohol-extracted supplements. But even then-don’t mix with meds.
The Bigger Picture: Why This Isn’t Going Away
The global kava market hit $117 million in 2022. Most sales happen online, bypassing any medical advice. Naturopathic doctors still recommend it-41% of them, according to a 2023 survey. But board-certified psychiatrists? Only 3% do.
Regulators are catching up. California issued formal warnings in May 2024. New York is pushing for mandatory liver toxicity labels. The FDA’s 2023 draft guidance calls for enhanced liver monitoring in kava trials. Research is underway at Oregon State University to see if traditional “noble” kava strains are safer than commercial varieties.
But until then, the risk remains. And it’s not worth it.
Can I take kava with a low dose of Xanax if I only use it occasionally?
No. Even occasional use with benzodiazepines like Xanax increases the risk of dangerous sedation and liver damage. There’s no safe threshold when combining kava with prescription sedatives. The interaction is dose-dependent and unpredictable due to inconsistent kava potency. It’s not worth the risk.
I’ve been taking kava for years with no issues. Am I safe?
Liver damage from kava can take months or even years to show up. Many people feel fine until their liver enzymes suddenly spike. Studies show 89% of patients with kava-induced liver injury reported fatigue and nausea months before diagnosis. If you’re taking any sedatives, alcohol, or have a history of liver problems, stop kava now-even if you feel fine.
Is kava tea safer than capsules or tinctures?
Yes, traditional water-based kava tea is significantly safer than alcohol or acetone extracts. The WHO found water extracts have 9 times fewer adverse events. But even tea isn’t risk-free if you’re on sedatives. The active kavalactones are still present. Avoid mixing any form of kava with prescription medications.
What should I tell my doctor if I’ve used kava?
Be specific: say you’ve taken kava, how often, in what form (capsule, tea, tincture), and for how long. Mention if you’ve combined it with any sedatives, alcohol, or sleep aids. Don’t say “I took a herbal supplement.” Many doctors don’t ask about kava-it’s not on standard intake forms. You need to volunteer it.
Are there any supplements that are safe to take with sedatives instead of kava?
Yes. Valerian root, magnesium glycinate, and melatonin have minimal interactions with sedatives. Cognitive Behavioral Therapy (CBT) is the most effective long-term solution for anxiety without any physical risks. If you need stronger help, talk to your doctor about FDA-approved medications like buspirone or hydroxyzine-they’re monitored, dosed precisely, and tested for safety.
Final Thought: Natural Doesn’t Mean Safe
Kava isn’t the villain. The real issue is the myth that “natural” equals harmless. Millions of people use kava without problems. But when it’s mixed with sedatives, the risk skyrockets-and the damage can be irreversible. Your liver doesn’t scream before it fails. It whispers. Fatigue. Nausea. A slight yellow tint. If you’re taking any kind of sedative, don’t ignore those whispers. Stop kava. Talk to your doctor. Choose safer paths. Your liver will thank you.

robert cardy solano
November 19, 2025 AT 17:03Man, I’ve been taking kava for years with my nightly tea-no issues. But now that I’m on low-dose lorazepam for anxiety, I’m gonna pause it. Better safe than sorry. My liver’s not a guinea pig.
Rebecca Cosenza
November 21, 2025 AT 05:16Stop. Just stop. Natural doesn’t mean safe. You’re playing Russian roulette with your liver. 😔
Pawan Jamwal
November 22, 2025 AT 00:38USA is so paranoid about everything. In India, we’ve used kava-like herbs for centuries with zero problems. Your FDA is just scared of natural alternatives. 🤷♂️
Nick Naylor
November 23, 2025 AT 16:05Let’s be clear: kava is a CYP2D6/CYP3A4 inhibitor-period. When combined with benzodiazepines, it causes pharmacokinetic drug-drug interactions that elevate plasma concentrations beyond therapeutic thresholds, increasing the risk of respiratory depression and hepatotoxicity. This isn’t anecdotal-it’s pharmacology 101. And no, ‘I’ve been fine for years’ doesn’t negate enzyme suppression. You’re not immune-you’re just not symptomatic yet.
Brianna Groleau
November 24, 2025 AT 09:28I grew up in Fiji-kava was part of our Sunday gatherings. We’d sit in a circle, drink from the tanoa, talk, laugh, feel calm. It wasn’t about escaping-it was about connection. But I get it: the commercial stuff sold in the U.S. is a totally different beast. Alcohol extracts, unregulated doses, no transparency. That’s not kava-it’s a chemical gamble. Please, if you’re gonna use it, go for traditional water-based, and never mix it with meds. We lost too many of our elders to liver disease already. Don’t repeat that here.
Rusty Thomas
November 26, 2025 AT 04:06So I took kava with Xanax once-just one time-and woke up on the floor at 3 a.m. with my dog licking my face. I thought I was dead. Turns out, I was just out cold for 8 hours. My doctor said I got lucky. Now I tell everyone: if you’re on sedatives, kava is the equivalent of putting a match to a gas can. 🔥💀
Sarah Swiatek
November 26, 2025 AT 04:23It’s funny how we treat pharmaceuticals like science and herbal stuff like witchcraft. But here’s the truth: both can kill you. The difference? One comes with a warning label, and the other comes with a $12 bottle from a website that says ‘100% Pure Kava (Guaranteed to Chill You Out)’ and has zero lab reports. You wouldn’t take a random pill from a stranger’s backpack-why take a random capsule labeled ‘kava extract’? The real villain isn’t kava. It’s the unregulated supplement industry. And the people who think ‘natural’ means ‘no consequences.’
Dave Wooldridge
November 27, 2025 AT 15:24THEY’RE HIDING THE TRUTH! The FDA banned kava because Big Pharma doesn’t want you to know you can chill without a prescription! They’ve been suppressing research since 2002! Look at the WHO report-they admit water-based kava is safe! But the FDA? They’re in bed with Pfizer! They want you addicted to pills so you keep paying! I’ve got my own kava farm in Oregon-no chemicals, no alcohol extracts, just noble strain, hand-pounded. You think I’m paranoid? Check the 2024 California report-they’re already backtracking on their own warnings! THEY’RE LYING TO YOU!!
Lemmy Coco
November 28, 2025 AT 12:45hey i used kava for like 6 months with my zoloft and never had any issues but then i got a cold and took benadryl and just… passed out for 3 hours? my roomate had to wake me up. i thought i was having a stroke. i stopped kava after that. still feel weird about it. maybe i was just lucky? idk. i dont know if i should tell my doc i used it? i feel like they’ll judge me. 😅
Bill Camp
November 29, 2025 AT 07:59Let me get this straight-you’re telling me a plant root from the Pacific is more dangerous than opioids, alcohol, or antidepressants? We’re banning kava but letting Big Pharma sell you daily doses of benzodiazepines that cause addiction, withdrawal, and cognitive decline? That’s not safety-that’s hypocrisy. And you know what? I’ve got a cousin who’s a liver specialist-he says kava-induced liver injury is rarer than being struck by lightning. But hey, if you wanna live in fear of every herb, go ahead. I’ll be over here, breathing.