When you’re managing a chronic autoimmune condition like rheumatoid arthritis, psoriasis, or severe eczema, the idea of swapping daily injections for a simple pill can feel like a game-changer. That’s exactly what JAK inhibitors offer. These oral drugs, also known as JAK inhibitors, are reshaping how we treat inflammatory diseases-not by blocking single proteins like biologics do, but by stepping in at the cellular level to shut down entire signaling pathways that drive inflammation.
How JAK Inhibitors Actually Work
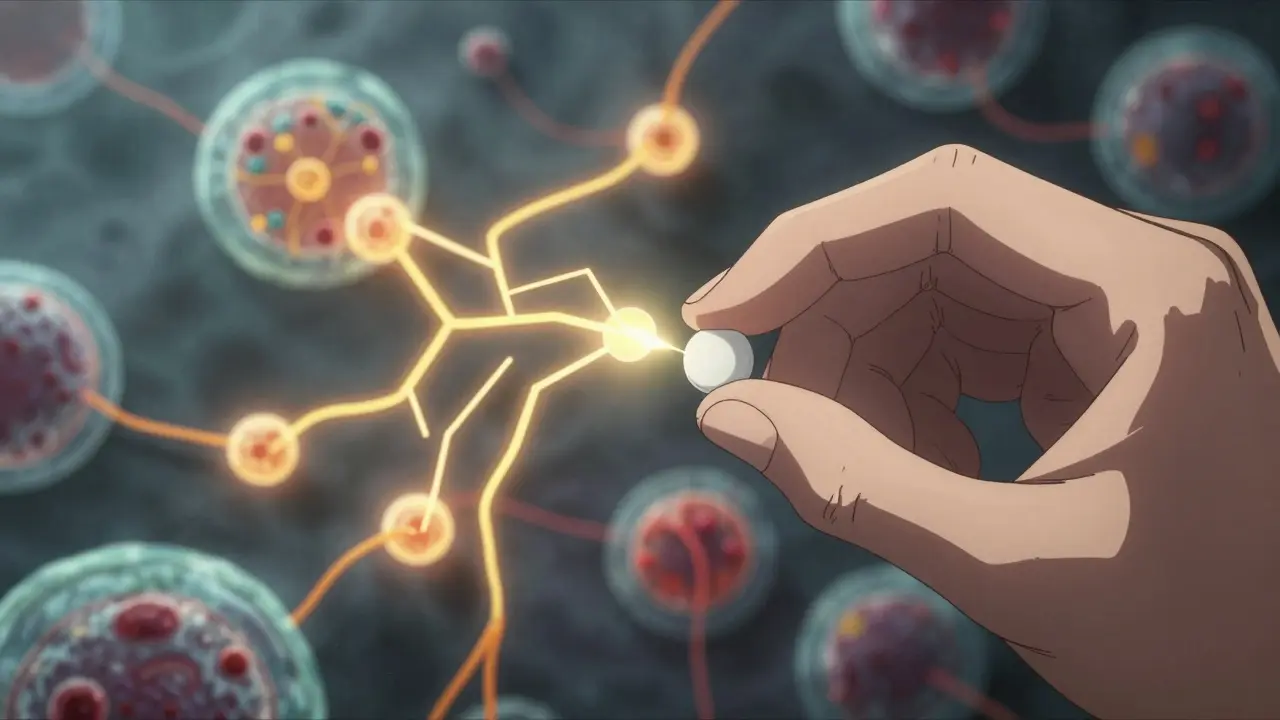
Inside your immune cells, there’s a chain reaction called the JAK-STAT pathway. When cytokines-signaling molecules like IL-6 or IL-23-bind to receptors on the cell surface, they activate enzymes called Janus kinases (JAKs). These JAKs then turn on STAT proteins, which zip into the nucleus and flip genetic switches that produce more inflammation. JAK inhibitors block this process by sticking to the active site of JAK enzymes, preventing them from sending the signal. It’s like cutting the wires before the alarm goes off.
There are four types of JAKs: JAK1, JAK2, JAK3, and TYK2. Each one connects to different cytokines. That’s why some drugs are designed to be more selective. For example, upadacitinib targets JAK1 with high precision (it’s 72 times more likely to bind JAK1 than JAK2), while older drugs like tofacitinib hit multiple JAKs at once. Ritlecitinib goes even further-it forms a permanent bond with JAK3 by attaching to a specific cysteine residue, making its effect longer-lasting. This selectivity matters because it can mean fewer side effects.
Which Conditions Are Treated?
Originally approved for rheumatoid arthritis in 2012, JAK inhibitors have quickly expanded into other areas. Today, they’re used for:
- Rheumatoid arthritis (tofacitinib, baricitinib, upadacitinib)
- Psoriatic arthritis (upadacitinib, baricitinib)
- Atopic dermatitis (abrocitinib, upadacitinib)
- Psoriasis (upadacitinib)
- Alopecia areata (ritlecitinib, deuruxolitinib)
Deuruxolitinib, approved in June 2024 for hair loss due to alopecia areata, is the newest addition. Patients report visible regrowth within weeks-something many never saw with steroids or topical treatments. For people with multiple conditions-say, rheumatoid arthritis and psoriasis-JAK inhibitors can treat both at once, reducing the need for multiple medications.
Why They’re Popular (and Why Some Doctors Are Wary)
The biggest appeal? Convenience. No more weekly injections. No cold storage. Just a pill you can take with breakfast. Studies show symptom relief often starts in 2-4 weeks, compared to 8-12 weeks with biologics like adalimumab. In one survey of over 1,200 patients, 92% preferred oral pills over shots, and 68% noticed improvement within two weeks.
But there’s a catch. Because JAK inhibitors affect broad signaling pathways-not just one cytokine-they can interfere with normal immune functions too. The FDA added black box warnings in January 2022 after the ORAL Surveillance trial showed higher rates of serious infections, heart attacks, strokes, blood clots, and cancer in patients taking tofacitinib compared to TNF blockers. The risk wasn’t huge for everyone-but it was real for those over 50 with heart disease or a history of smoking or cancer.
European guidelines now strictly limit JAK inhibitors to patients under 65 without cardiovascular risks. In the U.S., about 32% of rheumatologists still prescribe them as first-line after methotrexate, but in Europe, that number drops to 18%. The difference? A more cautious approach to long-term safety.
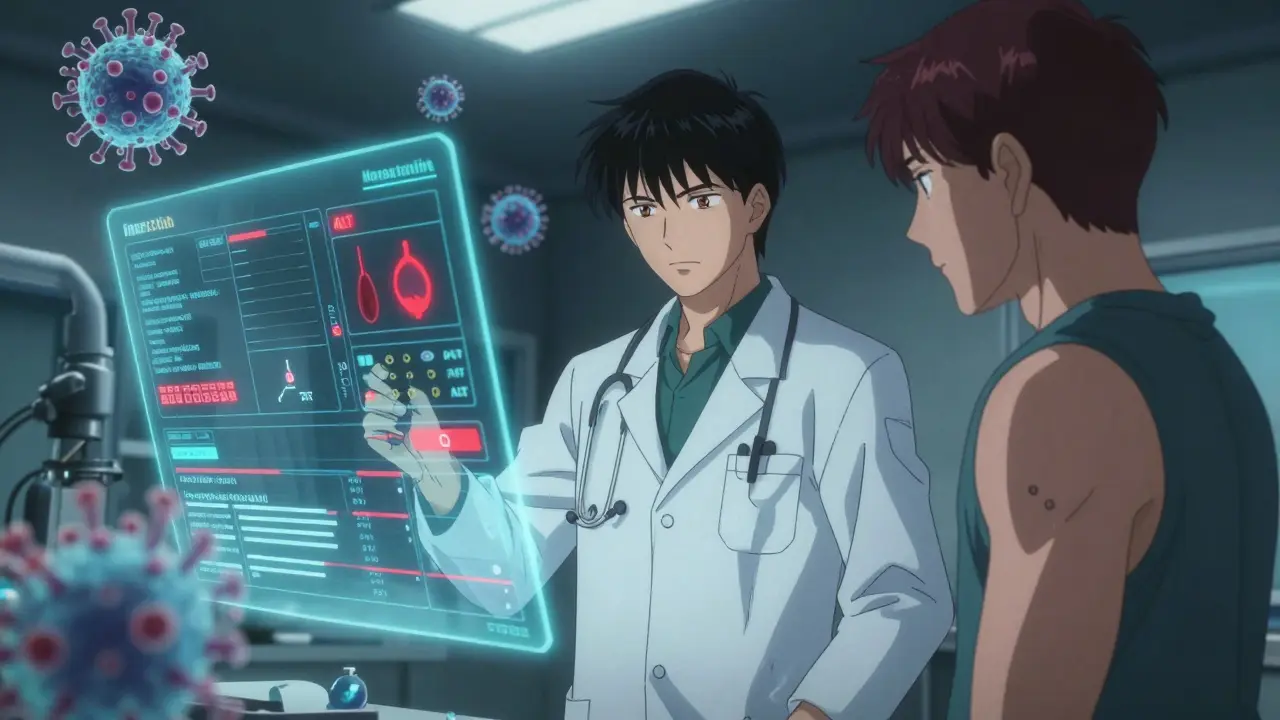
What You Must Monitor-And How Often
Taking a JAK inhibitor isn’t like taking a painkiller. You need regular blood tests. The American College of Rheumatology recommends:
- Baseline tests: Complete blood count, liver enzymes, lipid panel, TB screening, and hepatitis B/C testing.
- Every 3 months for the first year: Repeat CBC, liver enzymes, lipids, and kidney function.
- Every 6 months after that: Continue monitoring if stable.
Here’s what doctors watch for:
- Lymphocyte count: If it drops below 500 cells/μL, you’ll need to stop the drug. Low lymphocytes mean higher infection risk.
- Hemoglobin: Below 8 g/dL means anemia-a known side effect of JAK2 inhibition.
- Liver enzymes (ALT/AST): More than 3 times the upper limit means possible liver stress.
- LDL cholesterol: Many patients see a spike-sometimes 20-30 mg/dL higher. If it goes above 190 mg/dL, statins are usually added.
Herpes zoster (shingles) is another big concern. About 23% of users report reactivation, compared to just 3% on biologics. That’s why the EMA recommends getting the shingles vaccine at least 4 weeks before starting treatment. But in practice, only about 32% of European clinics manage to do this-often because patients are in too much pain to wait.
Real Patient Stories: Relief and Risk
One Reddit user, u/RhuemWarrior, shared: “Abrocitinib cleared my eczema in 10 days-but gave me shingles twice. Now I’m on daily antivirals. I’m grateful for the skin relief, but I’m scared of what’s next.”
Another patient on HealthUnlocked wrote: “After failing three biologics, baricitinib cut my swollen joints from 18 to 2 in six weeks. The $15 co-pay increase? Worth it.”
These stories aren’t outliers. In clinical trials, upadacitinib showed a 71% response rate (ACR20) in rheumatoid arthritis patients at 12 weeks-nearly double the placebo rate. But the same trial also reported a 3.5% incidence of serious infections over 12 months.
The Future: Better, Safer, More Selective
The next wave of JAK inhibitors is focused on precision. Brepocitinib, a TYK2/JAK1 inhibitor currently in phase 3 trials, is designed to avoid JAK2 entirely-potentially reducing anemia and blood clot risks. Deucravacitinib, already approved for psoriasis, works differently: it doesn’t block the ATP site. Instead, it binds to a regulatory region (JH2), making it more selective and possibly safer.
Industry analysts predict JAK inhibitors will capture 35% of the moderate-to-severe atopic dermatitis market by 2027. But long-term viability is still in question. A 2024 Medscape survey found 62% of rheumatologists would switch patients to newer biologics if they were equally effective but safer.
For now, JAK inhibitors are powerful tools-but they’re not for everyone. They work best for patients who need fast, oral relief and who can commit to regular monitoring. For those with heart disease, a history of cancer, or who can’t stick to blood tests, biologics or other options may still be the safer bet.
What’s Next for You?
If you’re considering a JAK inhibitor, ask your doctor:
- Am I at higher risk for heart disease, blood clots, or cancer?
- Have I been screened for TB and hepatitis?
- Will I need a shingles vaccine before starting?
- How often will I need blood tests-and who will track the results?
- What happens if my cholesterol or lymphocyte count goes off track?
There’s no one-size-fits-all answer. But with the right monitoring, JAK inhibitors can be life-changing. The key isn’t just taking the pill-it’s staying on top of the checks that keep you safe while you heal.
Are JAK inhibitors safe for long-term use?
Long-term safety depends on individual risk factors. Studies show increased risks of serious infections, blood clots, heart events, and certain cancers-especially in patients over 50 with cardiovascular disease or a history of smoking or cancer. Regular monitoring and strict patient selection are critical. For low-risk patients, the benefits often outweigh the risks, but ongoing surveillance is non-negotiable.
How do JAK inhibitors compare to biologics like Humira or Enbrel?
JAK inhibitors are taken orally, while biologics require injections or infusions. JAK inhibitors often work faster-symptom relief in 2-4 weeks versus 8-12 weeks for biologics. They also target multiple cytokines at once, which can help with multiple conditions. But biologics are more targeted, which usually means fewer systemic side effects. JAK inhibitors carry black box warnings for heart events and cancer that biologics don’t, making them riskier for certain patients.
Can I get the shingles vaccine while on a JAK inhibitor?
No. Live vaccines like Shingrix are not recommended while taking JAK inhibitors because your immune system is suppressed. The vaccine should be given at least 4 weeks before starting treatment. If you’re already on the drug, you can get the non-live recombinant zoster vaccine (Shingrix) but only under close medical supervision. Many clinics miss this step, putting patients at higher risk for shingles reactivation.
Do JAK inhibitors cause weight gain or hair loss?
Weight gain isn’t a direct side effect of JAK inhibitors, but improved appetite and reduced inflammation can lead to weight changes. Hair loss is not caused by these drugs-in fact, they’re used to treat it. Ritlecitinib and deuruxolitinib are FDA-approved for alopecia areata and have shown significant hair regrowth in clinical trials. Any hair loss while on treatment should be evaluated for other causes, like thyroid issues or stress.
What happens if I stop taking a JAK inhibitor?
Symptoms often return within weeks after stopping. Unlike some biologics, JAK inhibitors don’t typically induce long-term remission after discontinuation. If you stop due to side effects, your doctor may switch you to another JAK inhibitor or a biologic. Never stop abruptly without medical guidance-sudden withdrawal can trigger flare-ups. Some patients need to restart at a lower dose to re-establish tolerance.
Are JAK inhibitors covered by insurance?
Most insurance plans cover JAK inhibitors, but they often require prior authorization and step therapy-meaning you must try methotrexate or a biologic first. Out-of-pocket costs can range from $10 to $15 per month with good coverage, but without insurance, they can exceed $5,000 per month. Specialty pharmacies handle most prescriptions, and manufacturer assistance programs are widely available for eligible patients.
Retha Dungga
January 1, 2026 AT 06:10Jenny Salmingo
January 1, 2026 AT 18:07Brady K.
January 2, 2026 AT 06:47Kayla Kliphardt
January 3, 2026 AT 12:17John Chapman
January 5, 2026 AT 12:03Urvi Patel
January 7, 2026 AT 00:52Robb Rice
January 8, 2026 AT 10:01Darren Pearson
January 8, 2026 AT 23:58Stewart Smith
January 10, 2026 AT 12:13Aaron Bales
January 11, 2026 AT 21:42Lawver Stanton
January 13, 2026 AT 20:21Sara Stinnett
January 14, 2026 AT 18:30linda permata sari
January 15, 2026 AT 23:28