Every year, thousands of people end up in the hospital with liver damage-not from alcohol, not from viruses, but from something they thought was safe: a common painkiller. Acetaminophen, the active ingredient in Tylenol and dozens of prescription pain meds, is one of the most widely used drugs in the world. But when it’s mixed with opioids like hydrocodone or oxycodone in combination products, the risk of accidental overdose skyrockets. And most people don’t even realize they’re in danger.
Why Combination Products Are Riskier Than You Think
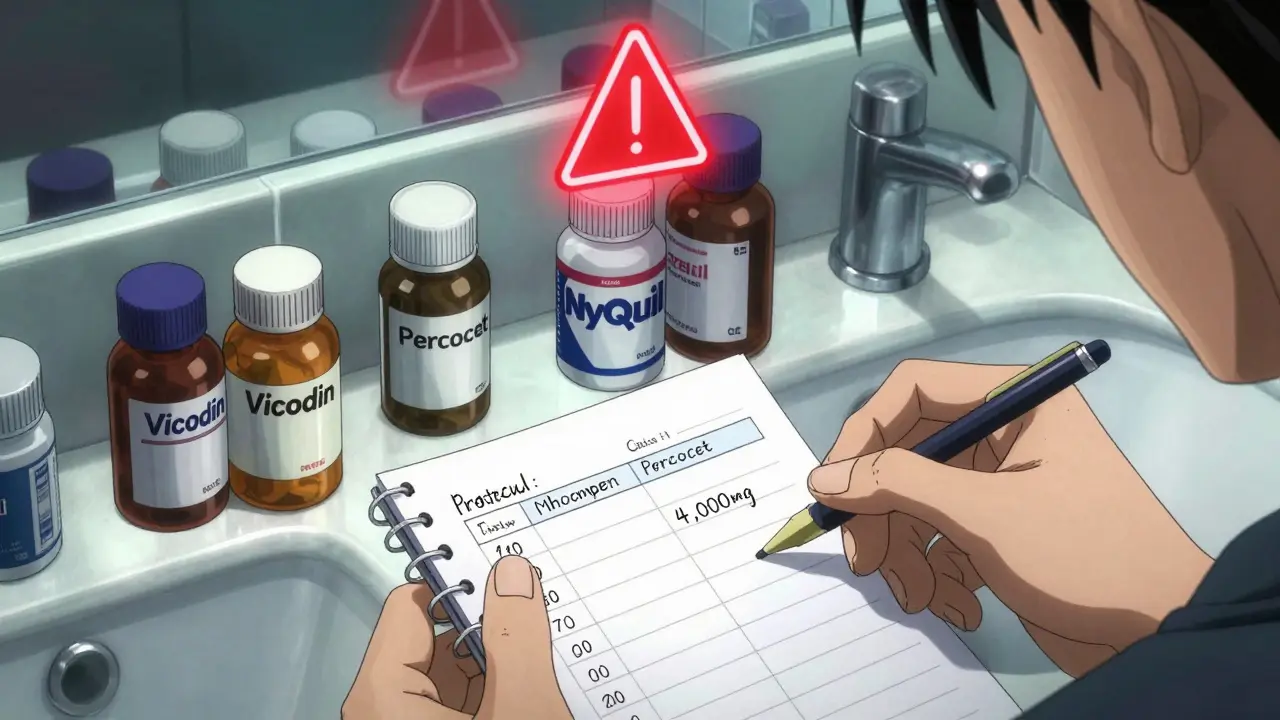
You might take Vicodin for a bad back, or Percocet after surgery, and think you’re just managing pain. But every pill contains acetaminophen-usually 325 mg per tablet. If you also take Tylenol for a headache, or a cold medicine like NyQuil, you’re stacking doses without knowing it. The safe daily limit for acetaminophen is 4,000 mg for most adults. That’s just 12 regular-strength Tylenol tablets. But with combination products, you can hit that limit in just four or five pills. And if you’re taking more than one type of combination drug? You’re already past the edge.In the U.S., nearly 40% of unintentional acetaminophen overdoses come from these combo pills, according to FDA data from 2011. Even after the FDA forced manufacturers to cap acetaminophen at 325 mg per dose in 2014, a 2019 study in Hepatology found that combo products still caused 27% of all acetaminophen-related liver injuries. And 68% of those cases were accidental.
The problem isn’t just the dose-it’s the confusion. A 2021 Consumer Reports survey found that only 37% of people knew acetaminophen was the main ingredient in Tylenol. Just 28% knew the maximum daily dose. On Reddit’s r/Pharmacy, a 2022 thread asking if people realized their painkillers had acetaminophen got over 1,200 responses. Two-thirds admitted they’d taken multiple acetaminophen-containing meds at once.
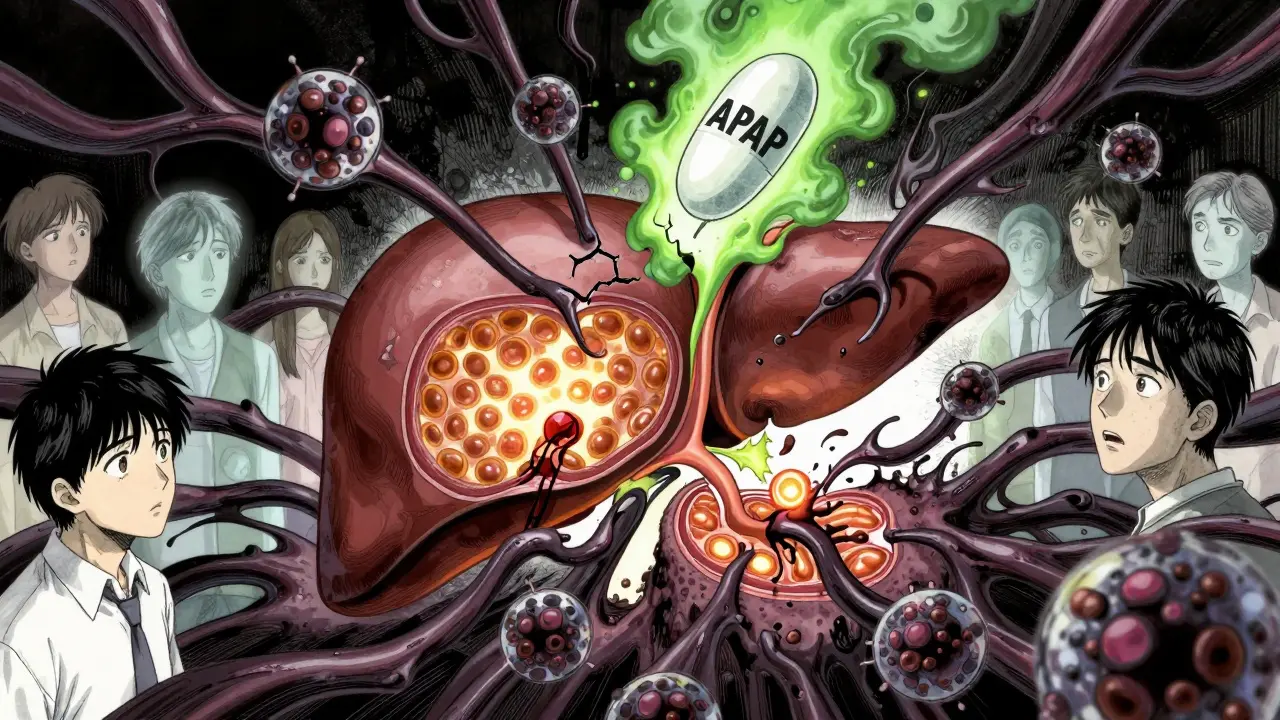
How Acetaminophen Actually Damages the Liver
Your liver normally breaks down acetaminophen safely using two main pathways: glucuronidation and sulfation. But when you take too much, those pathways get overwhelmed. The excess acetaminophen gets processed by a different enzyme-CYP2E1-which turns it into a toxic byproduct called NAPQI.NAPQI is dangerous because it eats through your liver’s natural defense: glutathione. Once glutathione drops below 30% of normal levels, NAPQI starts attacking liver cells. It damages mitochondria, the energy factories inside your cells. This triggers a chain reaction: oxidative stress, inflammation, and cell death. Without treatment, this can lead to acute liver failure within days.
What makes this worse is that you won’t feel sick right away. Many people don’t notice symptoms until 24 to 48 hours after taking too much. By then, the damage is already done. That’s why prevention isn’t just smart-it’s life-saving.
What You Can Do to Stay Safe
The best way to avoid liver injury is to stop the overdose before it starts. Here’s how:- Read every label, every time. Look for “acetaminophen,” “APAP,” or “paracetamol” on the ingredient list. It’s in cold medicines, sleep aids, migraine pills, and even some cough syrups. If you’re taking more than one medication, add up the acetaminophen content. Don’t guess-calculate.
- Never take more than one acetaminophen product at once. Even if one is prescription and the other is over-the-counter, they both add up. If your doctor prescribes hydrocodone/acetaminophen, stop taking Tylenol or any other acetaminophen-containing product unless your doctor says it’s okay.
- Know your daily limit. For most healthy adults, don’t exceed 3,000 mg per day if you drink alcohol regularly, have liver disease, or are underweight. The standard 4,000 mg limit is too high for many people. When in doubt, go lower.
- Use a medication tracker. Write down every pill you take, including doses and times. Apps like MyTherapy or the new FDA-backed barcode scanner app (currently in beta) can scan your pills and automatically track your acetaminophen intake across all medications.
- Ask your pharmacist. Pharmacists are trained to catch these mistakes. When you pick up a new prescription, ask: “Does this contain acetaminophen? And am I already taking anything else with it?” A 2021 study showed pharmacist-led counseling reduced unintentional overdoses by 41%.
Who’s at Highest Risk?
Some people are more vulnerable-even at lower doses. These groups need to be extra careful:- People who drink alcohol regularly. Alcohol depletes glutathione and activates the CYP2E1 enzyme, making liver damage more likely. Even one drink a day can increase your risk.
- People with malnutrition or eating disorders. Low protein intake means lower glutathione levels. Fasting or extreme dieting can put you at risk even with normal doses.
- Older adults and people with liver disease. Your liver processes drugs slower as you age. If you already have fatty liver or hepatitis, your tolerance drops dramatically.
- Non-English speakers. A 2020 study found Spanish-speaking patients had 2.3 times higher risk of accidental overdose due to language barriers in medication labels. Always ask for translated medication guides-FDA provides them in 14 languages.
What to Do If You Think You’ve Taken Too Much
If you’ve taken more than the safe dose-even if you feel fine-act fast. Don’t wait for symptoms. Go to the ER or call Poison Control immediately.The antidote is N-acetylcysteine (NAC). It works by restoring glutathione and protecting mitochondria. If given within 8 hours of overdose, it reduces liver injury by nearly half. Even after 24 hours, it still helps. The Rumack-Matthew nomogram is the tool doctors use to decide if you need NAC based on your blood acetaminophen level and when you took it.
In 2021, the FDA approved fomepizole as a new treatment option. It blocks the enzyme that turns acetaminophen into NAPQI. When used with NAC, it can reduce severe liver injury by 32% if given within 12 hours.
Don’t rely on home remedies. Inducing vomiting or drinking milk won’t help. Only NAC can reverse the damage.
What’s Changing in 2026?
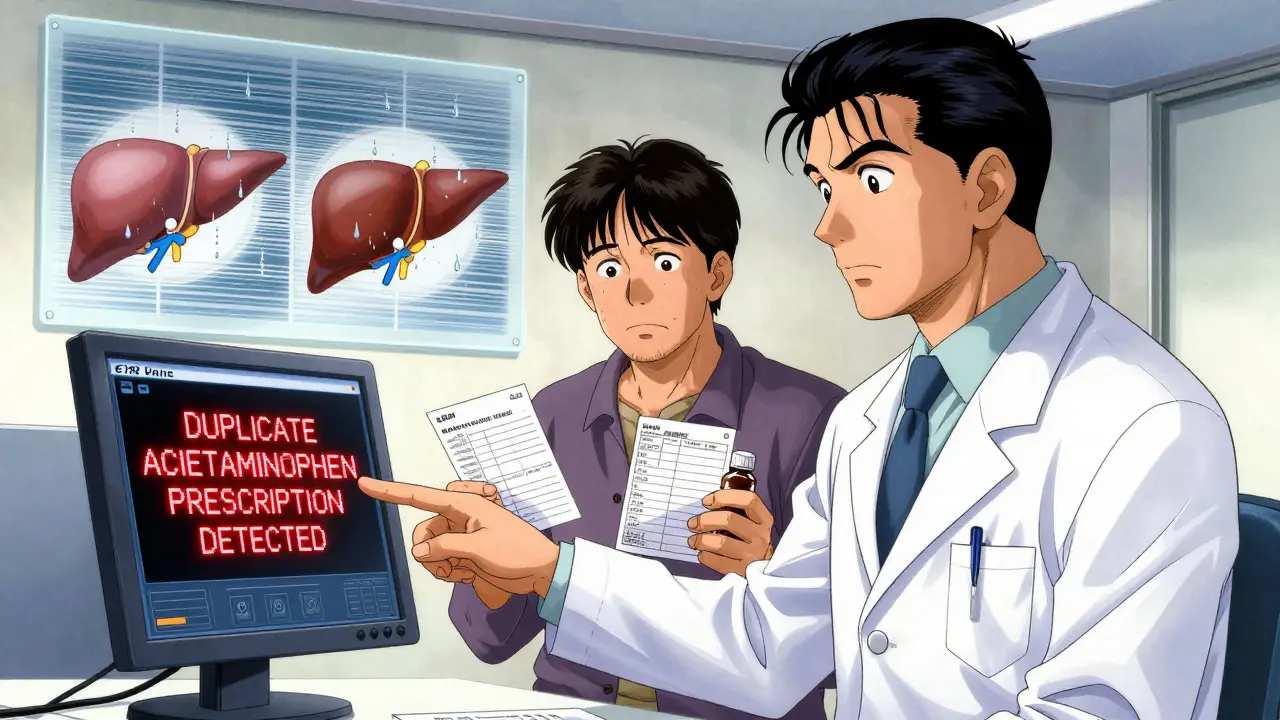
Regulations and tools are improving. Since 2014, FDA-mandated bold red labels on combo products have cut unintentional overdoses by 29%. In 2023, the FDA started considering lowering the maximum dose in OTC acetaminophen from 1,000 mg to 650 mg per tablet. That would make it harder to accidentally overdose with just a few pills.Pharmacies are now required to use EHR systems that flag duplicate acetaminophen prescriptions. Over 87% of Epic EHR systems do this automatically. And new extended-release NAC tablets, approved in early 2023, last 12 hours instead of 4-making treatment easier to complete at home.
Researchers are also exploring natural protectants like emodin (from rhubarb) and sulforaphane (from broccoli sprouts), which activate the body’s own antioxidant systems. But experts warn: these aren’t replacements for safe use. They’re potential backups, not excuses to ignore the rules.
Final Warning: Don’t Trust Your Memory
The biggest mistake people make? Thinking they’ll remember what they took. You won’t. Stress, pain, fatigue, and medication side effects cloud your judgment. That’s why you need systems-not willpower.Keep a written list of every medication you take. Store it in your phone, wallet, or on your fridge. Share it with a family member. Ask your pharmacist to review it every time you refill a prescription. If you’re unsure, don’t take it. Call your doctor. Wait. Double-check.
Acetaminophen is safe when used correctly. But in combination products, it’s one of the most dangerous drugs in your medicine cabinet. You don’t need to avoid it. You just need to know what you’re taking-and how much.
Can I take acetaminophen if I drink alcohol?
If you drink alcohol regularly-even just one drink a day-you should limit acetaminophen to no more than 2,000-3,000 mg per day. Alcohol increases the production of the toxic metabolite NAPQI and lowers your liver’s protective glutathione levels. Mixing the two raises your risk of liver damage even at normal doses. If you drink heavily or have liver disease, avoid acetaminophen entirely unless your doctor approves it.
Is it safe to take Tylenol with a prescription painkiller?
No, unless your doctor specifically says so. Most prescription painkillers like Vicodin, Percocet, and Darvocet already contain acetaminophen. Taking Tylenol on top of that can easily push you over the 4,000 mg daily limit. Always check the active ingredients on the prescription label. If it says “acetaminophen” or “APAP,” don’t take any other acetaminophen-containing product.
How do I know if I’ve taken too much acetaminophen?
You might not feel anything for the first 24 hours. Early signs include nausea, vomiting, loss of appetite, and fatigue. By day two or three, you may develop pain in your upper right abdomen, jaundice (yellow skin or eyes), dark urine, or confusion. These are signs of liver damage. If you suspect an overdose-even if you feel fine-go to the ER immediately. Don’t wait for symptoms.
Can I use NAC at home to prevent liver damage?
No. N-acetylcysteine (NAC) is a medical treatment, not a preventive supplement. It must be given under medical supervision, usually intravenously. Taking NAC pills from the store won’t protect you from an overdose. They’re not strong enough and won’t reach the liver fast enough. Only use NAC if prescribed by a doctor after a confirmed overdose.
Are there safer alternatives to acetaminophen combination products?
Yes. For pain, ask your doctor about non-acetaminophen options like tramadol, codeine (without acetaminophen), or non-opioid alternatives like gabapentin or NSAIDs (if you don’t have kidney or stomach issues). For fever or mild pain, ibuprofen or naproxen may be safer-though they come with their own risks. Always discuss alternatives with your doctor before switching.
If you’re currently taking a combination painkiller, take five minutes today to check every medication in your cabinet. Write down each one that contains acetaminophen. Add up the total. If you’re over 3,000 mg, talk to your doctor. Your liver won’t warn you before it’s too late-but you can.
Susan Arlene
January 6, 2026 AT 03:01Tom Swinton
January 6, 2026 AT 22:53Joann Absi
January 8, 2026 AT 12:42Jeane Hendrix
January 9, 2026 AT 16:33Vinayak Naik
January 10, 2026 AT 12:05Indra Triawan
January 10, 2026 AT 13:14Melanie Clark
January 10, 2026 AT 14:07Mukesh Pareek
January 11, 2026 AT 23:55Matt Beck
January 12, 2026 AT 18:17Kelly Beck
January 13, 2026 AT 17:41Katie Schoen
January 14, 2026 AT 05:47Tiffany Adjei - Opong
January 15, 2026 AT 09:59Stuart Shield
January 17, 2026 AT 01:38Lily Lilyy
January 18, 2026 AT 03:38Ashley S
January 18, 2026 AT 08:42