Why a medication review isn’t just another doctor’s visit
If you’re taking five or more medications - prescription, over-the-counter, vitamins, or herbal supplements - you’re not just managing health. You’re managing complexity. A medication review isn’t a check-up. It’s a safety check. It’s where your doctor or pharmacist looks at every pill, patch, inhaler, and drop you take and asks: Is this still helping you? And more importantly: Is it safe?
Many people think they’re doing fine as long as they don’t feel bad. But side effects can creep in slowly. A medication that worked fine a year ago might now be making you dizzy, tired, or confused. Or worse - it could be reacting with something else you’re taking. That’s why annual medication reviews are now standard in primary care. In some places, if you skip your review, your prescriptions get cut off. Not as punishment. As protection.
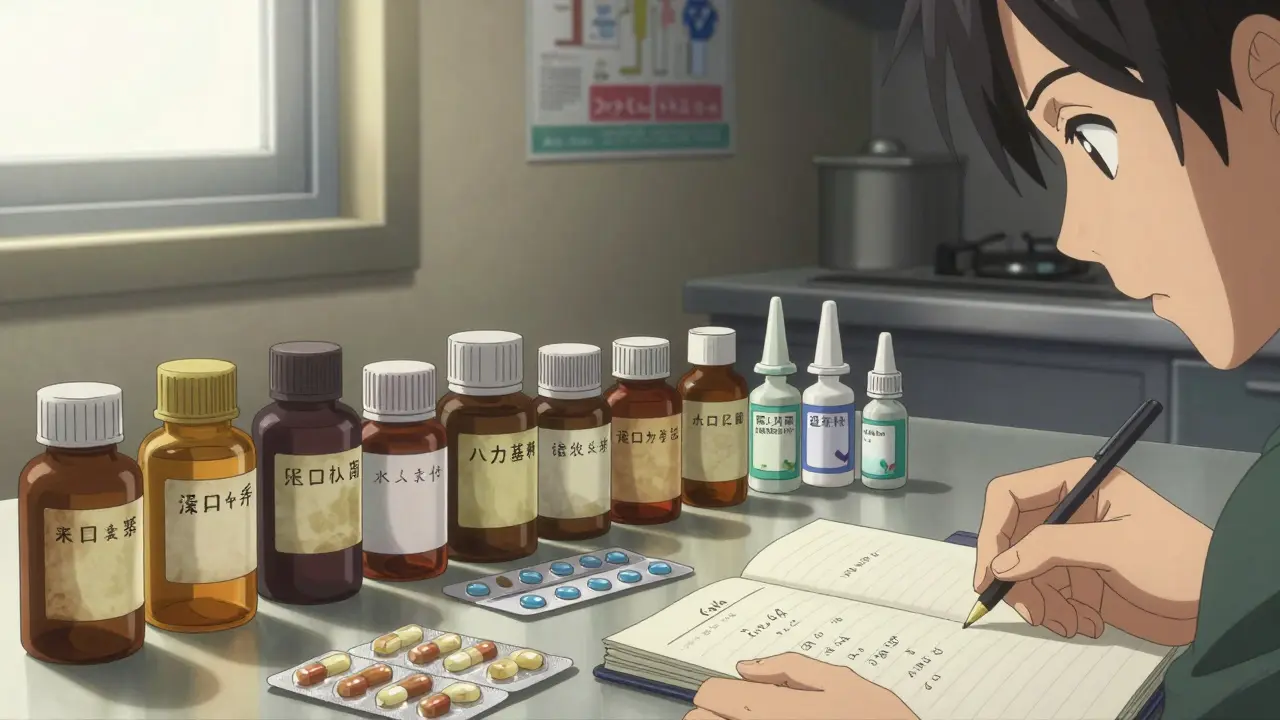
What you need to bring - everything
Don’t rely on memory. Don’t say, “I think I take two of those.” Bring the actual bottles. Every single one.
- Prescription medications (even ones you haven’t taken in months)
- Over-the-counter drugs like ibuprofen, antacids, or sleep aids
- Vitamins, minerals, and supplements - yes, even the ones from the health food store
- Herbal remedies, teas, or tinctures
- Inhalers, creams, eye drops, patches
- Any medication you stopped taking and why
Some people think, “Oh, I don’t take that anymore,” and leave it at home. But if you stopped it because it made you sick, that’s critical information. Your provider needs to know what didn’t work - and why.
Bring the physical bottles. Not just a list. Why? Because labels show the exact dosage, expiration date, and prescribing doctor. A pill bottle says “Take one tablet twice daily.” But if your memory says “once a day,” that’s a red flag. The label doesn’t lie.
Write down the details - not just the names
On a piece of paper, or in your phone notes, list each medication with these details:
- Medication name (brand or generic)
- Dosage (e.g., 10 mg, 5 mL, one inhalation)
- Frequency (e.g., once daily, every 6 hours, as needed)
- Reason you take it (e.g., “for high blood pressure,” “for joint pain,” “for anxiety”)
- Prescribing provider (e.g., Dr. Lee, Cardiologist)
- Side effects you’ve noticed (e.g., “dry mouth,” “feels shaky after lunch,” “sleepy after dinner”)
Don’t skip the side effects. Even small ones. If you’ve been feeling more tired than usual since starting a new pill, write it down. That could be the key to changing your whole regimen.
Know your goals - what do you want from this visit?
A medication review isn’t just about what your provider wants to fix. It’s about what you want to improve.
Ask yourself:
- Is there a pill I wish I didn’t have to take every day?
- Do I forget to take something because the schedule is too complicated?
- Are any of these medicines making daily life harder - like causing dizziness when I walk, or making me feel nauseous after meals?
- Do I feel like I’m taking too many things for one problem?
Write down two or three things you want to talk about. Example: “I want to see if I can reduce my pain pills because they make me foggy in the morning.” Or: “I’m scared of the blood thinner because I bruise easily.”
When you speak up, your provider can’t guess what’s bothering you. You have to say it.
Special cases: Parkinson’s, elderly, or telehealth
If you have Parkinson’s disease, timing matters more than ever. Medications like levodopa work in narrow windows. If you take them 30 minutes late, the effect drops. Write down exact times: “Levodopa at 7:00 AM, 11:00 AM, 3:00 PM, 7:00 PM.” This is especially critical for phone or video visits - your provider can’t see the bottle.
If you’re older or have memory issues, ask a family member to come with you. Or have them help you make the list ahead of time. Some clinics offer home visits if you can’t travel. Don’t assume you’re stuck - ask.
For telehealth appointments: test your video or phone connection before the day. Have your medications laid out on a table so you can hold them up to the camera. Make sure you’re in a quiet place. No background noise. No distractions. This isn’t a casual chat - it’s a medical safety check.
What happens during the appointment
Your provider will likely start by asking you to walk through your list. They’ll check for:
- Overlapping drugs - two medicines that do the same thing
- Drug interactions - one medicine making another stronger or weaker
- Unnecessary meds - something you were prescribed for a short-term issue that never got stopped
- Dosage issues - too high, too low, or wrong timing
- Side effects you didn’t connect to your meds
They might suggest stopping one, lowering a dose, switching to a different one, or adding something new. Don’t be surprised if they say, “You don’t need this anymore.” Many people are taking pills they don’t need - sometimes for years.
They’ll also ask: “Do you understand why you take each one?” If you can’t explain it, that’s a problem. You should know what each pill does. If you don’t, ask again. No judgment.
What if you’re told to stop a medication?
Some medications can’t be stopped cold turkey. Blood pressure pills, antidepressants, seizure drugs - these need to be tapered slowly. If your provider says to stop one, ask: “How do I do that safely?” Get it in writing. Ask for a schedule: “Reduce by 25% every two weeks.”
Don’t assume you can just quit. That can cause serious withdrawal symptoms or rebound effects. If you’re unsure, ask for a follow-up in two weeks to check how you’re doing.
What happens if you skip your review
In some clinics, after three reminders with no response, your prescriptions are limited. After that, they stop refilling them entirely. Not to punish you. Because without knowing what you’re taking, they can’t safely prescribe anything new.
Imagine you get sick and go to the ER. They don’t know if you’re on blood thinners, heart meds, or diabetes drugs. That’s dangerous. Your provider’s hands are tied until you complete the review.
After the appointment - what to do next
Ask for a written summary. Not just a verbal update. Get a list of:
- Medications you’re still taking
- Medications you’re stopping or changing
- New doses or schedules
- Follow-up plan
Update your personal medication list right away. Share it with your family or caregiver. Put a copy in your wallet or phone. Keep it current.
If you’re still confused, call back. Don’t wait. A quick question now can prevent a hospital trip later.
Final reminder: This isn’t optional
Medication reviews aren’t a luxury. They’re a lifeline. Especially as you age, or if you’re managing multiple conditions. Every pill you take has a reason - but that reason can change. What helped last year might hurt you this year.
Preparing for your review takes 30 minutes. That’s less time than scrolling through social media. But it could save you from a fall, a hospital stay, or a dangerous interaction.
Bring your bottles. Write down your concerns. Speak up. You’re not just a patient. You’re the most important person in the room.
Hanna Spittel
January 2, 2026 AT 01:02Urvi Patel
January 2, 2026 AT 17:03Emma Hooper
January 3, 2026 AT 07:21Robb Rice
January 5, 2026 AT 00:10Deepika D
January 6, 2026 AT 20:18Bennett Ryynanen
January 7, 2026 AT 18:06Chandreson Chandreas
January 9, 2026 AT 15:52Retha Dungga
January 10, 2026 AT 16:37linda permata sari
January 11, 2026 AT 22:01Brandon Boyd
January 13, 2026 AT 01:41