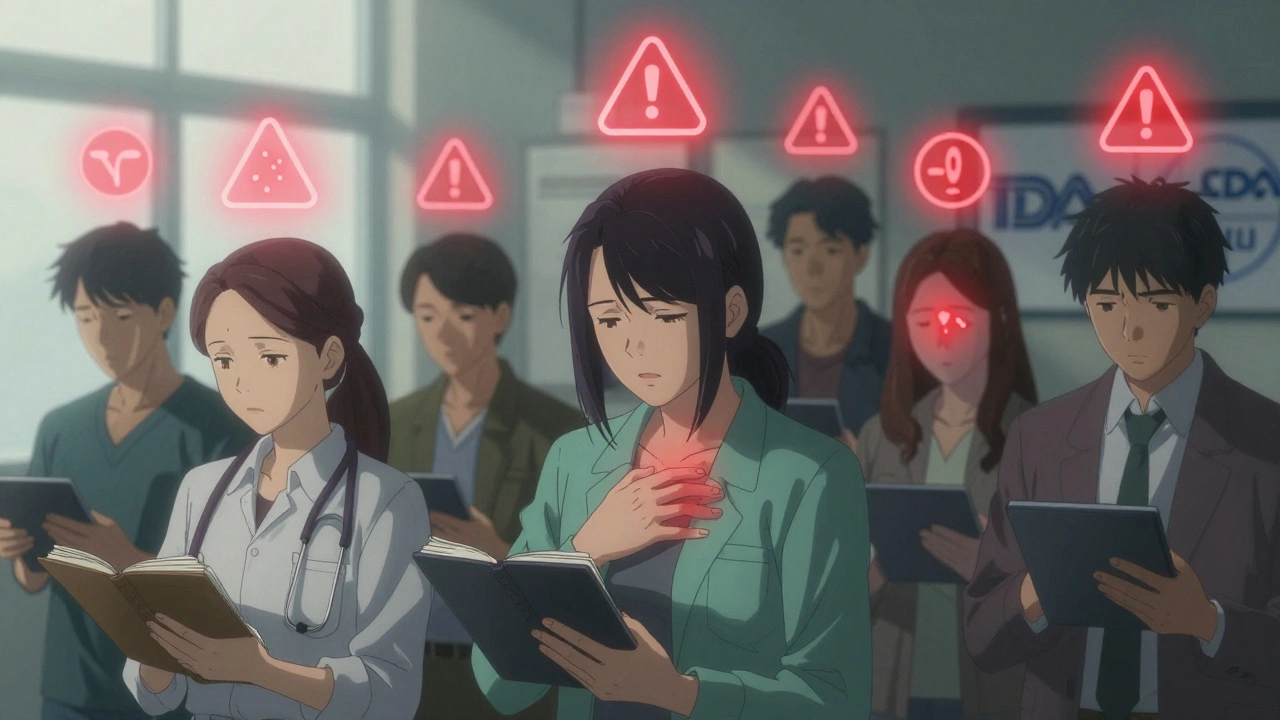
When you get a safety communication about a drug, medical device, or vaccine - whether it’s from the FDA, CDC, or your doctor - it’s not just a notice. It’s a call to action. These alerts aren’t sent out lightly. They come after real reports of side effects, malfunctions, or unexpected reactions. And if you’ve been exposed, your next step isn’t to panic. It’s to monitor your symptoms - carefully, consistently, and with a clear plan.
What Counts as a Safety Communication?
A safety communication isn’t a rumor or a social media post. It’s an official alert from a trusted health authority. The FDA issues them for medical devices that might fail, drugs that could cause rare but serious reactions, or vaccines with new safety data. The CDC uses them during outbreaks or after new exposure risks are identified. These aren’t vague warnings. They’re specific: "This batch of insulin pens has a higher risk of dosing errors," or "Patients taking Drug X have reported unexplained liver inflammation." When you get one, you’re being told: "Something unusual is happening. Watch for these signs." Your job isn’t to guess. It’s to track.Know What You’re Looking For
Not every symptom matters. Safety communications list exact signs to watch for. For example, if you’re told about a new risk of blood clots from a medication, you don’t need to track headaches or tiredness - unless they’re part of the alert. Focus only on what’s named. Common symptoms flagged in recent alerts include:- Unexplained bruising or bleeding
- Shortness of breath or chest pain
- Sudden swelling in legs or arms
- Severe rash, blistering, or peeling skin
- High fever with no other cause
- Changes in vision or speech
- Unusual fatigue or confusion
Choose Your Monitoring Method
You have two main options: active or passive monitoring. The choice depends on your risk level and what the alert recommends. Passive monitoring means you check yourself daily. You ask: "Do I have any of the listed symptoms?" You don’t wait for someone to call. You record what you feel - even if nothing’s wrong. This works well for low-risk situations, like a minor device update or a rare side effect affecting less than 1 in 10,000 people. Active monitoring means someone - your doctor, a public health team, or a digital system - checks in with you regularly. This is used for high-risk exposures, like after receiving a recalled implant or being in a known outbreak zone. You might get daily texts asking, "Any new fever?" or be asked to log symptoms in a secure app. Most people start with passive monitoring. But if you’re over 65, have chronic conditions, or live alone, active monitoring is safer. Don’t wait for someone to offer it - ask your provider.Use a Simple Tracking System
You don’t need fancy tech. But you do need consistency. Here’s what works:- Keep a notebook or digital note labeled "Safety Alert Tracker."
- Each day, write the date and note any symptoms - even if they’re mild.
- Use a 0-10 scale for severity: 0 = nothing, 5 = bothersome, 10 = unbearable.
- Include details: "Headache at 7 a.m., lasted 2 hours, didn’t respond to ibuprofen."
- Track medications, sleep, and diet - sometimes triggers aren’t obvious.

Know When to Act - and How
Monitoring isn’t just about logging. It’s about knowing when to call for help. If you notice any symptom listed in the alert, don’t wait. Don’t assume it’s "probably nothing." Contact your doctor or go to an urgent care center. Bring your tracker. Say: "I received a safety alert about [drug/device], and today I experienced [symptom]. Here’s what I’ve tracked." Use the SBAR method to communicate clearly:- Situation: "I’m calling because I have chest pain after taking Drug X."
- Background: "I got an FDA alert about this on March 10. I’ve been taking it for 12 days."
- Assessment: "I’ve had this pain for 4 hours. It’s a 7/10."
- Recommendation: "I need to be checked for possible heart inflammation."
What If You Miss a Day?
It happens. Life gets busy. If you forget to log a symptom one day, don’t panic. Just resume tracking the next day. But if you missed multiple days during a high-risk period - like after a recalled implant - call your provider. Say: "I missed tracking for three days. I’m concerned I might have missed a warning sign." Many people quit tracking because they feel guilty. Don’t. Monitoring is a tool - not a test. The goal isn’t perfection. It’s early detection.Don’t Ignore the Long Game
Most alerts ask for monitoring for 7 to 30 days. But some risks appear later. For example, a 2022 FDA alert on a blood pressure drug found liver damage appearing up to 6 months after starting. So, even after your official monitoring window ends, stay alert. Keep your tracker for at least 90 days. If you start feeling odd later - even if it’s unrelated - refer back. Sometimes symptoms connect in hindsight.What to Do If You’re Overwhelmed
Monitoring can feel exhausting. Especially if you’re juggling work, family, or chronic illness. You’re not alone. Ask for help:- Can a family member check in with you daily?
- Does your clinic offer a nurse hotline for alert-related questions?
- Can you set phone reminders to log symptoms?
Why This Matters - Beyond You
Monitoring isn’t just personal. It’s public health. When you track and report symptoms, you help researchers spot patterns. In 2021, early reports from patients monitoring after a certain vaccine led to the discovery of a rare heart inflammation risk - and saved lives by changing dosing guidelines. The CDC found that facilities with strong patient monitoring saw 37% fewer transmission events during outbreaks. Your tracking data helps protect others.What to Do After the Alert Expires
Once the monitoring period ends, don’t just delete your logs. Save them. Store them in your personal health record. You never know when a future doctor will need to know: "Did you ever have an unusual reaction to Drug Y?" If you had a serious reaction, report it to the FDA’s MedWatch program. It’s free, anonymous, and critical for future safety updates. You can file online at fda.gov/medwatch or call 1-800-FDA-1088.Final Thought: You’re the First Line of Defense
Doctors can’t monitor every patient every day. Devices can’t feel pain. Apps can’t know if your headache is new or normal. That’s where you come in. Safety communications aren’t meant to scare you. They’re meant to empower you. You have the power to catch problems early - before they become emergencies. You have the power to help others by sharing what you learn. And you have the power to stay calm, stay curious, and stay in control.Monitor. Record. Report. That’s it. You don’t need to be an expert. You just need to be attentive.
Annie Gardiner
December 7, 2025 AT 08:44Rashmi Gupta
December 9, 2025 AT 06:35Andrew Frazier
December 11, 2025 AT 03:28Kumar Shubhranshu
December 11, 2025 AT 19:11Mayur Panchamia
December 12, 2025 AT 17:40Nava Jothy
December 13, 2025 AT 13:06brenda olvera
December 15, 2025 AT 00:38Myles White
December 15, 2025 AT 02:57Ibrahim Yakubu
December 15, 2025 AT 16:11Chris Park
December 16, 2025 AT 14:54Saketh Sai Rachapudi
December 17, 2025 AT 11:54joanne humphreys
December 18, 2025 AT 16:09