When women start experiencing hot flashes, night sweats, or mood swings during menopause, hormone therapy can be one of the most effective ways to get relief. But not all hormone treatments are the same. The right combination depends on your body, your history, and what you’re trying to fix. For many, generic hormone therapy combinations offer the same results as brand-name drugs-at a fraction of the cost. Still, choosing the wrong one can increase risks you didn’t even know about.
Why Combination Therapy Matters
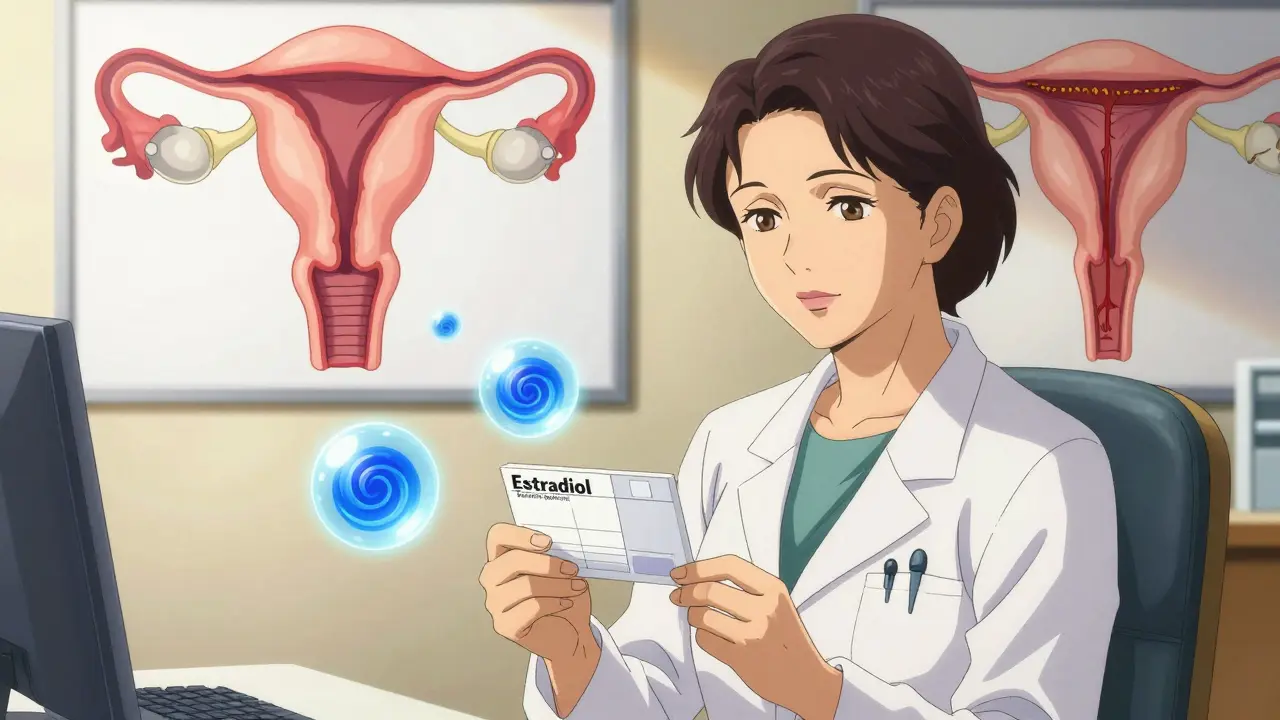
If you still have your uterus, you can’t take estrogen alone. It will cause the lining of your uterus to thicken, which can lead to cancer. That’s why doctors always pair estrogen with progestogen in women with an intact uterus. This combination protects the endometrium while still easing menopausal symptoms. For women who’ve had a hysterectomy, estrogen-only therapy is safe and often preferred. It’s simpler, has fewer side effects, and carries a lower risk of breast cancer than combined therapy. But if you haven’t had surgery, your treatment must include progestogen. The key is matching the right type and delivery method to your situation.Two Main Types of Combination Therapy
There are two main ways to combine estrogen and progestogen: sequential and continuous.- Sequential combined HRT is for women who are still having periods or just stopped recently. You take estrogen every day, then add progestogen for 10-14 days each month. This mimics your old cycle and often causes monthly bleeding-like a period. It’s designed to help women transition out of perimenopause.
- Continuous combined HRT is for women who haven’t had a period for a full year. You take both hormones every day, without breaks. This usually stops bleeding after a few months and is better for long-term use. It also lowers the risk of colon cancer by about 18% and type 2 diabetes by 21%, according to data from the Women’s Health Initiative.
The difference isn’t just timing-it’s safety. Taking the wrong type can lead to unexpected bleeding, confusion, or even unnecessary biopsies. Many women start on sequential therapy too late and end up with irregular spotting for months. That’s why timing matters as much as the drugs themselves.
Generic Options You Can Actually Trust
Generic hormone therapies are just as effective as branded ones. The FDA requires them to meet the same standards for strength, purity, and absorption. The big difference? Price.- Conjugated estrogens (like Premarin generics): Available in 0.3mg, 0.45mg, and 0.625mg tablets. Often prescribed for women starting therapy.
- Estradiol (like Estrace generics): Comes in 0.5mg and 1mg tablets. More similar to the estrogen your body naturally makes.
- Medroxyprogesterone acetate (like Provera generics): Used in 2.5mg, 5mg, and 10mg doses. A synthetic progestogen, common in older prescriptions.
But here’s something many don’t know: micronized progesterone (brand name Prometrium) is a natural form of progesterone. It’s not always generic, but it’s often cheaper than you think-and safer. Studies show it carries less breast cancer risk than synthetic progestins like medroxyprogesterone. For every year you use synthetic progestins, your breast cancer risk goes up by 2.7%. With micronized progesterone, it’s just 1.9%. That difference adds up over time.
Delivery Methods: Patches, Gels, or Pills?
How you take your hormones changes everything.- Oral tablets are the most common-but also the riskiest. They pass through your liver first, which increases clotting factors. That means a 2-3 times higher risk of blood clots and a 39% higher stroke risk if you’re over 60.
- Transdermal patches and gels deliver hormones through your skin. They skip the liver, so they don’t raise clotting risk the same way. The NHS and NIH both say these are safer for women with a history of clots, high blood pressure, or migraines with aura.
- Intrauterine systems (IUS), like the Mirena coil, release progestogen directly into the uterus. You still need estrogen in pill or patch form, but the IUS protects your lining with very low doses. Many women prefer this because it cuts bleeding and is effective for up to five years.
Transdermal options are growing fast in Europe-65% of prescriptions there are patches or gels. In the U.S., it’s still only 35%. Why? Cost and habit. But if you’re over 50 or have any risk factors for clots, switching to a patch or gel could be one of the smartest health moves you make.
Who Should Avoid Hormone Therapy?
HRT isn’t for everyone. The biggest red flags:- History of breast cancer
- History of blood clots, stroke, or heart attack
- Unexplained vaginal bleeding
- Liver disease
- Starting therapy after age 60 or more than 10 years after menopause
Doctors now agree: HRT is for symptom relief-not disease prevention. Taking it to protect your heart, bones, or brain doesn’t work. In fact, starting it late can do more harm than good. As one Houston-based specialist put it: ‘Throwing hormones at a 70-year-old woman with a history of heart disease? That’s dangerous.’
If you’re under 60 and within 10 years of your last period, the benefits usually outweigh the risks-especially if you choose transdermal estrogen and micronized progesterone. But if you’re older, or have other health issues, the balance flips.

What to Expect When You Start
Most women don’t feel better right away. It takes 3 to 6 months to find the right dose and delivery method. Side effects like breast tenderness, bloating, or mood swings are common at first-but they often fade. One of the most common surprises? Breakthrough bleeding. About 15-20% of women on continuous combined therapy will spot or bleed during the first six months. That’s normal. But if it lasts longer than that, you need to see your doctor. It could mean your dose is too low, or something else is going on.Also, don’t skip the follow-ups. Your needs change. A dose that worked at 52 might be too much at 58. Most guidelines now recommend reviewing your treatment every year after the first 3-5 years. You might be able to lower your dose-or even stop.
Cost and Access: What You Really Pay
In the U.S., generic HRT can cost anywhere from $4 to $40 a month, depending on your insurance and pharmacy. Patches and gels are usually more expensive than pills-but not always. Some Medicare Part D plans cover transdermal options at low copays. In the UK, most HRT is free with a prescription under the NHS.Generic versions of estradiol and micronized progesterone are widely available and often under $10 a month with coupons. GoodRx and SingleCare can cut your bill by half or more. Don’t assume the cheapest option is the worst. The most expensive brand isn’t always the best fit.
What’s New in 2026?
The field is evolving. A new transdermal patch combining estrogen and progesterone was approved by the FDA in late 2023. Early data suggests it may lower breast cancer risk compared to older oral combos. Research from the KEEPS study shows that starting transdermal estradiol within three years of menopause may actually protect your heart-not hurt it.Newer treatments like tissue-selective estrogen complexes (TSECs) and selective progesterone receptor modulators (SPRMs) are in late-stage trials. These aim to give symptom relief without the cancer risks. They’re not on the market yet, but they’re the future.
For now, the best approach is simple: start low, go slow, and pick the delivery method that fits your life and your risks. You don’t need to take hormones forever. Many women stop after 3-5 years, once hot flashes fade. Others stay on longer for quality of life. The key is making sure it’s still right for you-not just what you started with.
Can I take generic hormone therapy instead of brand-name?
Yes. Generic hormone therapies are required by the FDA to have the same active ingredients, strength, and absorption as brand-name versions. Estradiol, conjugated estrogens, and medroxyprogesterone acetate generics work just as well. The only difference is cost-generics often cost 80% less. Many women save hundreds a year by switching.
Is transdermal HRT safer than pills?
For most women, yes. Transdermal estrogen (patches, gels, sprays) doesn’t pass through the liver, so it doesn’t increase clotting factors the same way oral pills do. Studies show a 2-3 times lower risk of blood clots and stroke with transdermal methods. This is especially important for women over 50, those with migraines, high blood pressure, or a history of clots.
Why do I need progesterone with estrogen?
If you still have your uterus, estrogen alone causes the uterine lining to thicken. Over time, that can lead to endometrial hyperplasia-and eventually cancer. Progesterone prevents this by regularly shedding the lining. You don’t need it if you’ve had a hysterectomy. But if you haven’t, skipping progesterone is dangerous.
How long should I stay on hormone therapy?
There’s no fixed timeline. Most women take it for 3-5 years to manage symptoms. But if symptoms persist, it’s safe to continue at the lowest effective dose. The key is annual reviews. If you’re over 60 or started therapy more than 10 years after menopause, you should reconsider. Long-term use (5+ years) slightly increases breast cancer risk, but only by less than 1 in 1,000 per year.
Does HRT cause weight gain?
Not directly. Weight gain during menopause is usually due to aging, reduced muscle mass, and changes in metabolism-not hormones. Some women report water retention or bloating at first, but that usually goes away. If you’re gaining weight, focus on diet, movement, and sleep. Hormone therapy itself isn’t the culprit.
Can I use HRT if I’ve had breast cancer?
Generally, no. Most doctors avoid hormone therapy in women with a history of estrogen-receptor-positive breast cancer. Even low-dose or transdermal forms can stimulate cancer cells. There are rare exceptions, but only under strict supervision by an oncologist. Non-hormonal options like gabapentin, SSRIs, or lifestyle changes are safer alternatives.
What’s the best way to start HRT?
Start with the lowest dose possible and give it at least 3 months to work. If you’re still having periods, begin with sequential therapy. If you’re postmenopausal, start with continuous combined. Choose transdermal if you have any clotting risks. Always discuss your personal health history-especially blood pressure, cholesterol, and family cancer history-before starting.
Sangeeta Isaac
January 21, 2026 AT 02:10so like... i took generic estradiol for 6 months and still felt like a microwave set to 'low simmer'??? like why is my brain still on fire at 3am?? also why is my doctor acting like i'm asking for unicorn tears when i ask for a patch??
Rod Wheatley
January 21, 2026 AT 02:38THIS. I'm a nurse who's helped 37 women start HRT, and the #1 mistake? Starting oral pills without checking clotting risk. Transdermal is safer-period. If you're over 50, have migraines, or high BP? Skip the pill. Patches or gels. Full stop. Also-micronized progesterone over medroxy? Yes. It's not 'alternative medicine,' it's science. Studies show 1.9% vs 2.7% breast cancer risk per year. That's not a drop-it's a damn landslide.
And don't let Big Pharma scare you off generics. Estradiol 1mg generic? $7 at Walmart. Premarin? $120. Same molecule. Same FDA approval. Just cheaper. You're not 'settling.' You're being smart.
Also-yes, you need progesterone if you have a uterus. No, it's not 'overkill.' It's cancer prevention. Estrogen alone = endometrial cancer risk. Period. I've seen the biopsies. Don't gamble.
And if you're thinking 'I'll just wait till I'm 70 to start'-no. That's when it turns dangerous. The window is 60 or within 10 years of menopause. After that? You're not 'protecting' your heart-you're risking stroke. Trust the data, not the TikTok gurus.
And yes, HRT doesn't cause weight gain. That's just aging. Focus on protein, sleep, and walking. Not more hormones.
Start low. Go slow. Review yearly. You don't need this forever. But if you need it? Use it right.
Barbara Mahone
January 22, 2026 AT 11:11Thank you for writing this. I wish more doctors would explain the difference between sequential and continuous HRT. I was on sequential for 18 months after my last period and wondered why I was still bleeding like a teenager. Turned out I was way past perimenopause. Switched to continuous-no more monthly drama. Life changed.
Uju Megafu
January 22, 2026 AT 21:53Oh wow, so now we’re just supposed to trust Big Pharma’s generic pills? And who exactly approved these 'micronized progesterone' things? Are they even real? I heard the FDA is just a front for pharmaceutical lobbyists. And what about the 2023 patch? Did you know it’s being tested on women who don’t even know they’re pregnant? I’m not taking hormones until someone proves they’re not turning us into lab rats.
michelle Brownsea
January 24, 2026 AT 18:34Let me just say this: if you're taking HRT, you're not 'managing symptoms'-you're surrendering to a patriarchal medical system that tells women their bodies are broken. Hormones are not the answer. The answer is radical self-acceptance. Eat turmeric. Meditate. Walk barefoot. Let your body 'naturally' adjust. Why are we so afraid of aging? Why do we think we need to chemically reverse it? This isn't medicine-it's capitalism disguised as healthcare.
And don't get me started on 'transdermal'-that's just another way to make you pay more for the same thing. The real problem? Society doesn't value older women. Not hormones. Not patches. Not even micronized progesterone. Just respect.
Jarrod Flesch
January 25, 2026 AT 16:15Just wanted to say-switched to estradiol patch + micronized progesterone after 2 years of spotting and mood swings. 3 weeks later, I slept through the night for the first time since 2020. 😌 Also, my skin stopped looking like a dried-out peach. Worth every penny. And yes, generics are legit. I got mine for $9 with GoodRx. No drama. No BS. Just relief.
Andrew Rinaldi
January 26, 2026 AT 17:16I appreciate the nuance here. It’s easy to fall into extremes-either 'HRT is a miracle cure' or 'HRT is poison.' The truth is somewhere in the middle, and it’s deeply personal. What works for one body may harm another. The key is listening-not just to doctors, but to yourself. And giving yourself permission to stop, adjust, or pause. There’s no moral victory in staying on it 'just in case.'
Amber Lane
January 26, 2026 AT 21:34Micronized progesterone is safer. Period.
Kelly McRainey Moore
January 27, 2026 AT 06:06I started HRT at 53 and thought I was going to die from the side effects. Turns out I just needed a lower dose and a patch instead of pills. Took 4 months to find the right combo, but now I feel like me again. Not 'menopausal me.' Just me. 🌸
Melanie Pearson
January 28, 2026 AT 06:46It’s alarming how casually this article promotes hormone therapy as a benign solution. The WHI data is often misrepresented. Breast cancer risk, stroke, gallbladder disease-these are not trivial trade-offs. And now we’re being told to trust generics? The FDA approval process is a joke. Why aren’t we demanding non-hormonal alternatives? Why is the medical establishment so eager to chemically sedate women instead of addressing root causes like chronic stress, poor nutrition, and environmental toxins? This isn’t healthcare-it’s chemical compliance.
Ashok Sakra
January 29, 2026 AT 23:46My cousin took HRT and then got cancer. So I told my mom not to take it. Now she’s screaming all night and can’t sleep. What do I do? I don’t want her to die but I don’t want her to get cancer either. This is so confusing. Why can’t doctors just say what’s safe?
MAHENDRA MEGHWAL
January 31, 2026 AT 16:50As a physician practicing in rural India, I can attest that access to even basic generic HRT remains a challenge. Many women suffer in silence due to stigma, cost, or lack of education. This article, while comprehensive, assumes a level of healthcare infrastructure that does not exist for the majority of the global population. While the science is sound, the real issue is equity-not just dosage or delivery method. We need systemic change, not just pharmaceutical alternatives.
For those fortunate enough to have access: yes, transdermal estrogen and micronized progesterone are preferable. But for millions? The priority should be education, affordability, and destigmatization. A patch won’t help if you can’t reach a pharmacy.
Let us not mistake privilege for progress.
Gerard Jordan
February 2, 2026 AT 04:16Just wanted to say-thank you for the clear breakdown. I’m 56 and started HRT 2 years ago. Took me 6 months to find the right combo (estradiol patch + oral micronized progesterone). Now I’m sleeping, not crying during commercials, and actually enjoying my life again. 🙌 Also-yes, the bleeding in the first 6 months? Totally normal. Don’t panic. Just call your doc if it doesn’t settle. And yes, generics are fine. I save $200/month. That’s a vacation. 💸
Roisin Kelly
February 3, 2026 AT 18:34Okay but what if the hormones are secretly making me crazy? Like, I’ve been reading about how estrogen messes with serotonin and I swear I’ve been having thoughts I didn’t have before. Like… why do I suddenly want to quit my job and move to Iceland? Is that menopause or is that the pills??