Most people think hemorrhoids are just an embarrassing nuisance-but they’re actually a common medical condition affecting 75% of adults at some point in their lives. The real problem? Many don’t know the difference between internal and external hemorrhoids, or how to treat them properly. And that confusion leads to delayed care, unnecessary pain, and sometimes serious mistakes.
What Exactly Are Hemorrhoids?
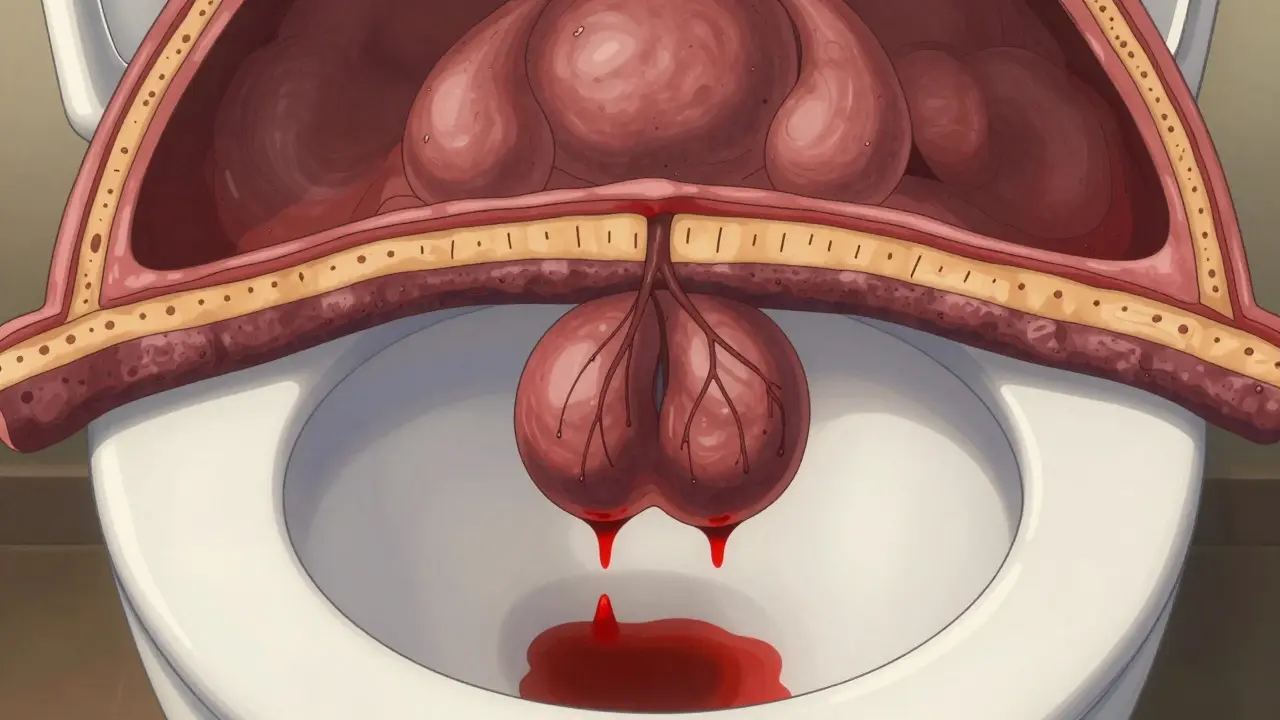
Hemorrhoids aren’t "swollen veins" in the way you might imagine. They’re normal vascular cushions inside and around your anus that help control stool passage. Think of them like shock absorbers for your rectum. But when pressure builds up-from straining, sitting too long, pregnancy, or chronic constipation-these cushions swell, inflame, and become painful or bleeding problems. The key to understanding them is location. Hemorrhoids are divided by the dentate line, a natural boundary inside the anal canal. Above it? Internal. Below it? External. And that tiny difference changes everything-especially how they feel and how they’re treated.Internal Hemorrhoids: Silent but Not Harmless
Internal hemorrhoids form inside the rectum, above the dentate line. The tissue there has no pain receptors. That’s why you might not feel them… until you do. Their main sign? Bright red blood. You’ll see it on toilet paper, in the bowl, or streaking your stool. No pain. No lump. Just bleeding. That’s why so many people ignore it-until the bleeding gets worse. Doctors grade internal hemorrhoids on a scale of I to IV:- Grade I: Bleeds but doesn’t prolapse (protrude)
- Grade II: Prolapses during bowel movements but pops back in on its own
- Grade III: Prolapses and needs to be pushed back in manually
- Grade IV: Stays outside permanently and can’t be pushed back
External Hemorrhoids: Painful and Hard to Ignore
External hemorrhoids form under the skin around the anus. That area is packed with nerves. So when they swell, you know it. Symptoms? Itching, burning, swelling, and a tender lump you can feel. Sometimes they look like a soft, skin-colored bump. Other times, they turn into a hard, purple or blue lump-that’s a thrombosed external hemorrhoid. It means a blood clot formed inside the vein. That’s when the pain hits hard: sharp, throbbing, and worse when you sit. Unlike internal hemorrhoids, external ones rarely bleed. But they can rupture and ooze, especially if you wipe too hard or strain. The pain peaks within 48 hours and can last for days. Many people delay treatment because they’re embarrassed. But waiting too long makes it worse.Can You Have Both at Once?
Yes. In fact, it’s common. Most people with hemorrhoids have a mix of internal and external types. That’s why symptoms can be confusing. You might bleed (internal) and also feel a painful lump (external). Or you think it’s just one thing-until the pain gets worse and you realize there’s more going on. This is why self-diagnosis is risky. A lot of people mistake anal fissures (tiny tears in the skin) for hemorrhoids. Fissures cause sharp, tearing pain during bowel movements-not itching or swelling. They don’t usually bleed much, but the pain is intense. Treat a fissure like a hemorrhoid? You’ll keep hurting.
What Causes Hemorrhoids?
It’s not just sitting too long on the toilet. Though that helps. The real triggers:- Chronic constipation and straining
- Chronic diarrhea
- Pregnancy (up to 35% of pregnant women get them)
- Obesity
- Heavy lifting
- Sitting for long periods (especially on hard surfaces)
Home Treatments That Actually Work
For mild cases, you don’t need surgery. Start here:- High-fiber diet: Aim for 25-30 grams daily. Think beans, oats, berries, broccoli, chia seeds. Most people get less than half that.
- Drink water: 8-10 glasses a day. Fiber without water makes constipation worse.
- Sitz baths: Sit in warm (not hot) water for 15-20 minutes, 2-3 times a day. It reduces swelling and soothes irritation.
- Witch hazel pads: Apply after bowel movements to reduce itching and inflammation.
- Hydrocortisone cream (1%): Use sparingly for itching. Don’t use for more than a week without checking with a doctor.
When You Need More Than Home Care
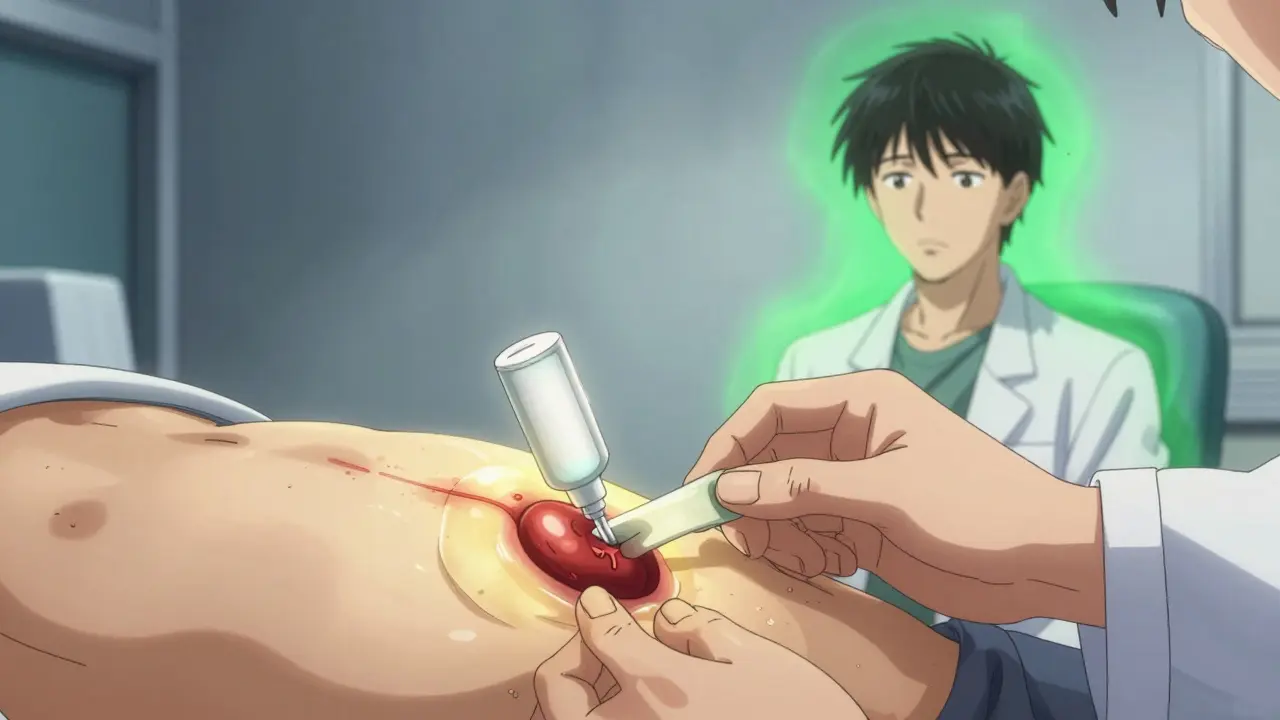
If home treatments don’t help in 1-2 weeks, or if you’re bleeding heavily, it’s time for medical help. For internal hemorrhoids, doctors have minimally invasive options:- Rubber band ligation: A tiny band is placed around the base of the hemorrhoid. It cuts off blood flow. The hemorrhoid shrinks and falls off in 5-7 days. Success rate: 90% for Grades I-III. You might feel pressure or mild cramping for a day or two.
- Sclerotherapy: A chemical is injected to shrink the vein. Less effective than banding but less painful.
- Infrared coagulation: Heat is used to scar the tissue and shrink the hemorrhoid. Good for smaller ones.
Surgery: When Nothing Else Works
If you have Grade IV hemorrhoids, recurrent problems, or severe pain that won’t quit, surgery may be needed.- Hemorrhoidectomy: The hemorrhoid is surgically removed. It’s the most effective treatment-95% success rate. But recovery takes 2-4 weeks. Pain is significant for the first week. You’ll need prescription pain meds.
- Stapled hemorrhoidopexy: Used for prolapsed internal hemorrhoids. The tissue is lifted and stapled back into place. Less pain than removal, but higher chance of recurrence.
What Not to Do
There’s a flood of online products promising "miracle cures" for hemorrhoids: creams, supplements, teas, devices. Most are useless. Some are dangerous. The American Gastroenterological Association and the American Society of Colon and Rectal Surgeons warn against products that claim to "cure" hemorrhoids overnight. They’re not regulated. They don’t work. And they delay real treatment. Also, never assume rectal bleeding is just hemorrhoids. It could be colon cancer, inflammatory bowel disease, or an infection. If you’re over 50, have a family history, or notice changes in bowel habits-get checked. Bleeding is never normal.Prevention Is the Real Cure
The best treatment is avoiding hemorrhoids in the first place.- Don’t sit on the toilet longer than 5 minutes.
- Don’t strain. If you don’t go after 5 minutes, get up and try later.
- Exercise regularly. Walking helps.
- Keep your weight healthy.
- For pregnant women: sleep on your left side, do pelvic floor exercises, and avoid constipation.
When to See a Doctor
Call your doctor if you have:- Bleeding that doesn’t stop or gets worse
- Pain that doesn’t improve after a week of home care
- A lump that won’t go away
- Dizziness, weakness, or signs of anemia (from blood loss)
- Changes in bowel habits, like diarrhea or constipation that lasts more than a few days
- Rectal bleeding for the first time after age 50
Can internal hemorrhoids turn into external ones?
No. Internal and external hemorrhoids form in different areas and have different tissue types. But internal hemorrhoids can prolapse and protrude outside the anus, which makes them feel like external ones. They’re still internally formed. A prolapsed hemorrhoid is an advanced stage of internal hemorrhoid, not a new type.
Do hemorrhoids go away on their own?
Mild cases often improve within a few days with home care-especially if you fix your diet and bowel habits. But the swollen veins don’t fully disappear unless treated. Without lifestyle changes, they’re likely to return. Think of it like a sprained ankle: rest helps, but if you keep running on it, it won’t heal.
Is hemorrhoid surgery painful?
Yes, especially after a traditional hemorrhoidectomy. Most patients need prescription pain medication for 7-10 days. The pain peaks around day 3 and gradually improves. Stapled procedures cause less pain but have a higher chance of recurrence. Rubber band ligation causes mild discomfort, not severe pain.
Can I exercise with hemorrhoids?
Absolutely-but avoid heavy lifting and straining. Walking, swimming, and light cardio help prevent constipation and improve circulation. Weightlifting, squats with heavy loads, and cycling on hard seats can worsen symptoms. Use a padded seat if you cycle, and always exhale during lifts, never hold your breath.
Why do I still bleed after treatment?
Bleeding after treatment can mean a few things: the hemorrhoid hasn’t fully healed, another one is developing, or it’s not a hemorrhoid at all. Persistent bleeding-even after successful banding or surgery-needs evaluation. It could signal an anal fissure, polyp, or something more serious like colorectal cancer. Don’t assume it’s just a recurrence.
If you’ve been living with hemorrhoids for months-or years-know this: you don’t have to suffer. The treatments work. The lifestyle changes make a difference. And seeing a doctor isn’t a sign of weakness-it’s the first step to feeling normal again.
Lance Nickie
January 12, 2026 AT 22:54hernioiods? more like hermoiods. i thought they were just from sitting too long on the toilet. turns out i’ve been doing it wrong my whole life lol.
vishnu priyanka
January 13, 2026 AT 00:43in india, we call them 'bubba's curse' - everyone knows someone who swears by a paste of neem and turmeric. no doctor, no surgery, just grandma’s wisdom. i’ve seen people walk it off like it’s a bad day at work. 🌿
Angel Tiestos lopez
January 13, 2026 AT 18:50sooo… hemorrhoids are basically our body’s way of saying ‘hey, you’re treating your butt like a stress ball’ 🤔. we sit, we strain, we scroll for hours like it’s a full-time job. maybe the real cure isn’t rubber bands or creams… it’s learning to chill the f*** out. 🧘♂️💩
Pankaj Singh
January 15, 2026 AT 10:46This article is a joke. You're telling people to eat fiber and drink water like it's 1998? Everyone knows the real cause is corporate greed - processed food, desk jobs, and pharmaceuticals hiding the truth. You think a sitz bath fixes anything? Wake up.
Scottie Baker
January 16, 2026 AT 18:54ok but why does it feel like someone is stabbing me with a rusty spoon every time i poop? i’ve been doing the fiber thing for 3 weeks and it’s still hell. who the f*** designed this body??
Anny Kaettano
January 17, 2026 AT 19:57Let’s normalize pelvic floor awareness - this isn’t just about hemorrhoids, it’s about biomechanics, neurology, and habitual tension patterns. You need diaphragmatic breathing, pelvic floor release techniques, and proper intra-abdominal pressure management. Fiber’s a start, but it’s not the whole system. 🧠🩹
Angel Molano
January 19, 2026 AT 12:54Stop being lazy. If you’re getting hemorrhoids, you’re just weak. Get off the couch. Stop eating junk. No one cares if you’re embarrassed - suffering is self-inflicted.
Trevor Davis
January 20, 2026 AT 07:22Hey, I just wanted to say - I’ve been dealing with this for 7 years. I thought I was alone. Reading this made me feel… seen. I started the sitz baths last week. It’s not magic, but it’s the first time in years I’ve slept through the night. Thanks for writing this. You’re a real one.
John Tran
January 21, 2026 AT 05:54Okay so like… imagine your anus is a tiny, overworked monk in a medieval monastery. It’s been sitting on a stone bench for 400 years, eating only gruel, and now it’s got a spiritual crisis because the monks above (your liver, your colon, your soul) keep sending it too much pressure and not enough grace. The rubber band ligation? That’s not medicine, that’s a divine intervention where the monk gets a new chair. And the hemorrhoidectomy? That’s the monk finally quitting and becoming a hermit in the woods. I’m not saying we should all go live in the forest… but maybe we should stop treating our butts like they’re made of concrete. 🏔️🙏
Milla Masliy
January 21, 2026 AT 06:39Thank you for this. I’m a nurse and I’ve seen so many patients delay care because they’re ashamed. This article is exactly what people need - clear, compassionate, and no shame. Keep sharing stuff like this. 💜