Medication Overuse Headache Calculator
How Often Are You Using Headache Medication?
The International Headache Society sets specific thresholds for safe use. Exceeding these may cause medication overuse headaches (MOH).
Ever taken painkillers for a headache, only to have it come back worse a few hours later? If you’ve been reaching for Advil, Excedrin, or even migraine meds like Imitrex more than a few days a week, you might not just have a bad headache-you could be triggering one yourself. This isn’t rare. Around 1 in 50 people in the U.S. suffer from medication overuse headaches, and most don’t even realize it’s happening. It’s not weakness. It’s not laziness. It’s a well-documented medical loop that traps people who are just trying to feel better.
What Exactly Is a Drug-Related Headache?
Medication overuse headache (MOH), sometimes called rebound headache, happens when you use headache medicine too often. Instead of stopping the pain, it starts causing more pain. The brain gets used to the drug, and when it wears off, your nervous system overreacts. That’s when the headache returns-often stronger than before.
This isn’t about occasional use. It’s about frequency. If you’re taking:
- Triptans (like Imitrex or Zomig) 10 or more days a month
- Opioids (oxycodone, tramadol) or butalbital meds (like Lanorinal) 10 or more days a month
- Combination pills (Excedrin, which has aspirin, acetaminophen, and caffeine) 15 or more days a month
- Simple NSAIDs like ibuprofen or naproxen 15 or more days a month
…you’re in the danger zone. The International Headache Society set these thresholds for a reason. Exceed them, and your brain’s pain system starts rewiring itself.
Who’s Most at Risk?
Women make up 70 to 80% of cases. Why? Not because they’re more prone to headaches-though migraine affects more women-but because they’re more likely to seek treatment early and use meds consistently. People with underlying migraine (affecting about 1 in 8 U.S. adults) or chronic tension-type headaches (affecting nearly 4 in 10 globally) are especially vulnerable. The problem isn’t the headache. It’s the cycle of treating it.
And here’s the twist: most people don’t think they’re overusing. They think, “I’m just taking what my doctor prescribed.” But even prescriptions can become the problem if used too often. Dr. Peter Goadsby, a leading headache specialist, says 85% of MOH cases happen despite following initial treatment guidelines. It’s a system failure, not a patient failure.
How Do You Know It’s Not Just a Bad Headache?
There are three red flags:
- You have headaches on 15 or more days a month for at least 3 months straight.
- Your headaches get worse when you try to stop or cut back on your meds.
- Your usual headache medicine doesn’t work like it used to-you need more, or it doesn’t last as long.
Most people with MOH describe their headaches as constant, dull, and worse in the morning. They might feel foggy, nauseous, or sensitive to light and sound-symptoms that mimic migraines or tension headaches. But the key difference? These headaches don’t respond to the same meds that used to help.
Keeping a headache diary for at least four weeks is the best way to spot the pattern. Write down:
- When the headache started
- How bad it was (1-10 scale)
- What medicine you took and when
- How long it lasted
After a month, look back. Do your headaches spike right after your last dose? That’s the telltale sign.
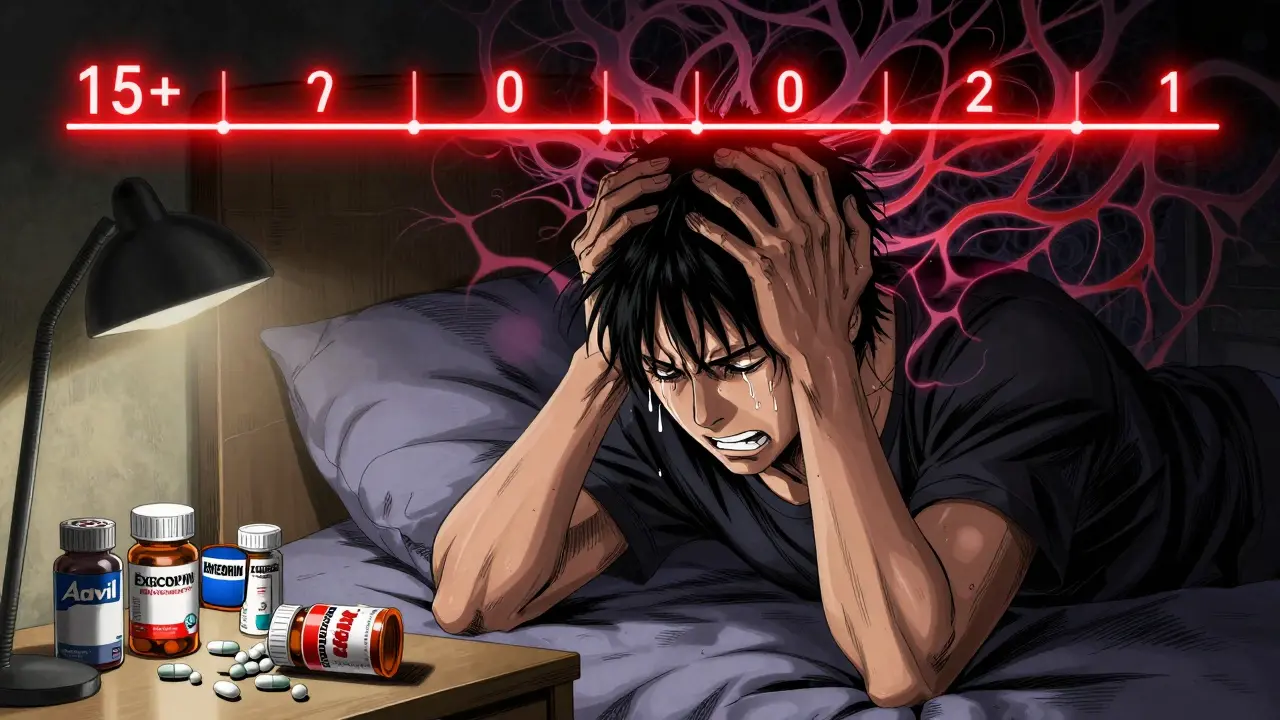
What Happens When You Stop?
Stopping the meds is the only way to break the cycle-but it’s not easy. Withdrawal symptoms are real and often brutal:
- Intensified headaches (92% of cases)
- Nausea (68%)
- Vomiting (42%)
- Low blood pressure (29%)
- Insomnia, anxiety, or depression
These symptoms usually peak between days 2 and 5 and start improving by week 2. But they can last up to 4 weeks. That’s why quitting cold turkey isn’t always safe-or smart.
For opioids or butalbital meds, stopping suddenly can cause seizures or dangerous drops in blood pressure. These cases often need medical supervision. For triptans or Excedrin, many people can quit at home-but only with a plan.
Mayo Clinic recommends:
- Stopping the overused medication completely (not tapering, unless it’s an opioid)
- Limiting rescue meds to no more than 2 days per week
- Using only non-overused pain relievers like acetaminophen (Tylenol) or low-dose NSAIDs
One Reddit user, u/HeadacheFreeNow, shared: “After 5 weeks off Excedrin, my headache days dropped from 28 to 9 per month.” That’s the kind of result people get when they stick with it.
What Comes After Withdrawal?
Stopping the meds is only half the battle. If you don’t treat the root cause, the headaches will come back. That’s why prevention is non-negotiable.
Doctors now recommend starting a preventive medication right after withdrawal. Options include:
- Topiramate (40-100 mg daily): Reduces migraine frequency by 50% in 60% of patients.
- Propranolol (80-160 mg daily): A beta-blocker that’s been used for decades with solid results.
- CGRP inhibitors (Aimovig, Ajovy, Emgality): Monthly injections that block a key migraine trigger. Studies show 50-60% of users cut their headache days in half.
There’s also a newer class of drugs called gepants-Ubrelvy, Nurtec ODT, Zavzpret. Unlike triptans, they don’t cause rebound headaches. They’re expensive (around $750 a month), but for people who’ve been stuck in the MOH cycle, they’re a game-changer. Prescription rates for these drugs have more than doubled since 2021.
And now, the FDA has approved atogepant (Qulipta) for preventive use in chronic migraine patients with MOH. It’s taken orally, works daily, and doesn’t carry the same overuse risk.
What About NSAIDs? Are They Safe?
This is where things get messy. The American Headache Society says taking ibuprofen or naproxen up to 15 days a month is fine. The European Headache Federation says 10 days is the limit. Why the difference? Because the science isn’t perfectly clear.
NSAIDs are less likely to cause MOH than opioids or triptans, but they’re not harmless. If you’re taking them daily for months, your body can still adapt-and your headaches can worsen. The key is moderation. If you’re using them for anything beyond occasional relief, talk to your doctor about alternatives.
What If You Can’t Quit?
Some people can’t stop on their own. That’s okay. You’re not alone. About 15-20% of people with MOH need inpatient care because withdrawal symptoms are too severe. Hospitals can manage nausea, blood pressure, and pain with IV fluids and controlled meds while your brain resets.
Outpatient programs work for most, but they require structure. You need:
- A clear stop date
- A written plan for rescue meds
- Follow-up visits every 1-2 weeks
- Support from someone who understands (a partner, friend, or support group)
One user on Reddit, u/PainPatient2023, wrote: “My clinic gave me no plan for the rebound week-I had to miss 3 days of work with vomiting and 24/7 headache.” That’s the kind of experience that turns people away from treatment. Don’t let that be you. Ask for a written plan. Demand support.
What’s Next? The Future of Headache Care
Science is moving fast. Researchers have identified 12 genetic markers linked to MOH susceptibility. In the next 5-10 years, a simple blood test might tell you if you’re at high risk before you even start taking meds.
There’s also research into non-drug treatments like transcranial magnetic stimulation (TMS), which uses magnets to calm overactive brain areas. The Migraine Research Foundation just funded a $2.5 million study on it.
And drugmakers are working on “smart” painkillers-medications engineered to avoid triggering rebound headaches at all. Dr. Richard Lipton predicts these could cut MOH rates by 40-50% in the next decade.
Bottom Line: You Can Break the Cycle
Drug-related headaches aren’t your fault. They’re a side effect of trying too hard to feel better. But they’re treatable. Thousands of people have walked out of this cycle. You can too.
Start by tracking your headaches and meds for four weeks. If you’re hitting those overuse numbers, talk to your doctor-not about more pills, but about how to stop safely. Don’t wait until you’re stuck with daily pain. The brain can heal. The headaches can fade. But only if you break the cycle.
It’s not about willpower. It’s about knowing the science-and using it.
Payson Mattes
December 24, 2025 AT 07:05Okay but have you ever heard that Big Pharma secretly designs painkillers to make you dependent? I mean, why else would they push these combo pills with caffeine and barbiturates? They know if you’re hooked, you’ll keep buying. I read a leaked memo once-there’s a whole division called ‘Rebound Engineering.’ They don’t care if you suffer, they just want your subscription. The FDA? Totally in on it. Just look at how slow they were to approve those new CGRP drugs-until the stock prices jumped.
Isaac Bonillo Alcaina
December 24, 2025 AT 09:22You misstate the diagnostic criteria. The IHS defines medication-overuse headache as occurring on ≥15 days per month for ≥3 months, not simply ‘more than a few days a week.’ Furthermore, the threshold for NSAIDs is 15 days, not 10. Your conflation of frequency thresholds undermines the credibility of the entire post. Precision matters-especially when discussing neurophysiological mechanisms.
Bhargav Patel
December 24, 2025 AT 14:35There is a profound irony in our relationship with pain. We seek to extinguish it, yet in doing so, we often amplify its presence. The body, in its wisdom, adapts-not as punishment, but as survival. To take a pill is to ask the nervous system to forget its own signals. But the nervous system remembers. It learns. And when the chemical crutch is withdrawn, it screams louder than before. Perhaps the real medicine is not in the tablet, but in the patience to let the body relearn its balance. This is not weakness. It is evolution in reverse.
Steven Mayer
December 25, 2025 AT 03:36The pharmacokinetics of triptan overuse involve 5-HT1B/1D receptor downregulation and central sensitization of trigeminovascular pathways. The glutamatergic cascade, particularly involving NMDA receptors in the trigeminal nucleus caudalis, becomes hyperexcitable. This isn't ‘rebound’-it’s neuroplastic maladaptation. Tapering opioids is mandatory due to GABAergic withdrawal, but NSAIDs don’t act on CNS receptors the same way-so the 15-day limit is arbitrary. Evidence-based thresholds require stratification by drug class, not blanket numbers.
Joe Jeter
December 25, 2025 AT 12:53So let me get this straight-you’re telling me the solution to taking medicine for pain is… to stop taking medicine for pain? Genius. Next you’ll tell me the cure for being cold is to stop wearing coats. If I have a headache every day, I’m not ‘overusing’-I’m just living with a broken body. Your ‘science’ ignores that some people’s brains don’t reset. Some of us are stuck. And now you want us to suffer through withdrawal like it’s a character-building exercise? Thanks, but I’ll keep my Excedrin.
Lu Jelonek
December 27, 2025 AT 11:59I’ve been helping patients with MOH for over a decade. The hardest part isn’t the withdrawal-it’s the guilt. They feel like failures because they ‘couldn’t just stop.’ But this isn’t addiction like opioids. It’s a physiological loop. I always tell them: You didn’t lose control. The medication rewired your brain. The fact that you’re reading this means you’re already on the path to healing. Start the diary. Don’t judge yourself. Just observe. The data will speak louder than shame.
Ademola Madehin
December 28, 2025 AT 19:02Brooooooo, I was on Excedrin for 3 years straight-2-3 a day. My head felt like a cinderblock. Then I went cold turkey. Vomited for 4 days. Cried in the shower. My wife left me for a week. But guess what? 8 months later? I haven’t had a headache in 2 weeks. I drink water. I sleep. I walk. I breathe. And I don’t take a damn pill unless I’m dying. You ain’t weak-you just ain’t tried the real fix yet.
suhani mathur
December 29, 2025 AT 18:54Oh wow, a 15-day limit for NSAIDs? That’s cute. In India, we have grandmas who take ibuprofen daily for arthritis and still jog at 70. Maybe the problem isn’t the drug-it’s that Western medicine treats pain like a bug to be eradicated, not a signal to be understood. We should be teaching people how to listen to their bodies, not how to outsource relief to a pill bottle. Also, CGRP inhibitors cost more than my rent. So yes, I’m sarcastic. Your ‘cure’ is only for the wealthy.
Diana Alime
December 30, 2025 AT 20:01i just took 3 advils and now my head hurts more??? like wtf?? i thought these were supposed to help?? i dont even know what im doing anymore. my doctor just gave me a script and said ‘take as needed’ but now i’m scared to take anything. why is this so complicated?? i just want to feel normal again. someone pls help.
Adarsh Dubey
December 31, 2025 AT 07:20It’s interesting how we treat pain as an enemy rather than a messenger. The body doesn’t lie. If you’re taking medication daily, it’s telling you something’s off-sleep, stress, posture, diet. The drugs silence the signal, but they don’t fix the source. I’ve seen people recover after switching to magnesium, hydration, and morning sunlight. No pills. No withdrawal. Just alignment. Maybe the real breakthrough isn’t a new drug-it’s a return to simplicity.
Jeffrey Frye
January 1, 2026 AT 03:00you say ‘break the cycle’ like it’s that easy. but what if you’re on 3 different meds because your migraines are triggered by weather, hormones, stress, and your damn cat sneezing? and your doc won’t prescribe anything stronger because ‘you’re overusing’? so now you’re stuck between a rock and a hard place. also-why is everyone on reddit acting like they’ve cured themselves? i’ve been trying for 7 years. my headache diary is 47 pages long. i’m not lazy. i’m just tired.