Calcitonin Dose Calculator for Bone Pain
This tool helps determine appropriate calcitonin dosing based on clinical condition, administration route, and pain severity. Always consult clinical guidelines and monitor calcium levels.
Quick Takeaways
- Calcitonin is a natural hormone that lowers blood calcium and can blunt bone‑derived pain.
- It is most useful for acute pain from metastatic lesions, recent fractures, and Paget’s disease.
- Administered as a nasal spray or sub‑cutaneous injection, typical doses range from 100‑200 IU daily.
- Side‑effects are usually mild (nasal irritation, nausea) but long‑term use can raise antibodies.
- Guidelines counsel short‑term treatment (2‑4 weeks) and careful monitoring of calcium levels.
calcitonin bone pain management blends endocrinology with palliative care. Below we unpack what calcitonin is, why it eases bone pain, and how clinicians can use it safely.
What Is Calcitonin?
When you first hear the name, think of a hormone made by the thyroid’s parathyroid C‑cells.Calcitonin helps regulate calcium by lowering blood levels and inhibiting bone resorption. It was isolated in the 1960s and quickly became a therapeutic option for conditions where bone turnover is too high.
Unlike the more famous parathyroid hormone (PTH), calcitonin’s action is short‑lived. It binds to receptors on osteoclasts-the cells that break down bone-and tells them to slow down. The result? Less calcium released into the bloodstream and a calmer bone environment.
How Calcitonin Relieves Bone Pain
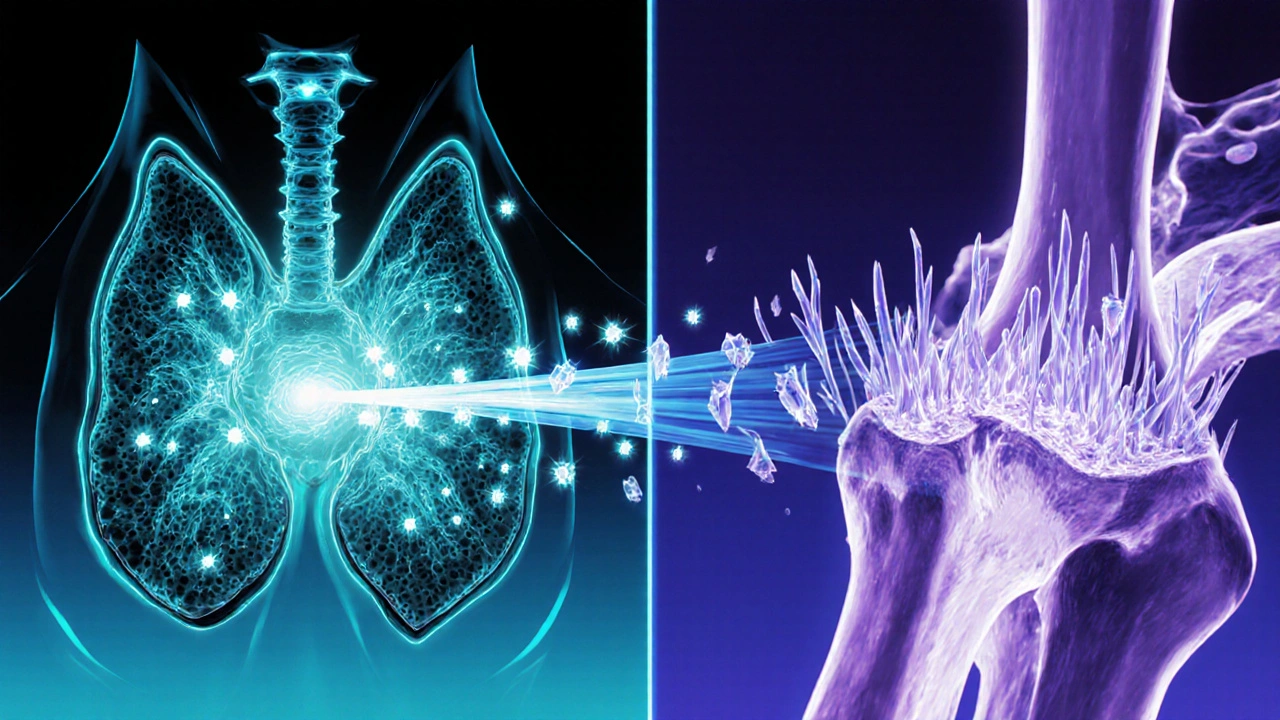
Bone pain isn’t just a simple ache; it’s a signal from constantly remodeling bone tissue. In diseases like metastatic cancer, tumors release substances that over‑activate osteoclasts, creating micro‑fractures and inflammatory mediators. Calcitonin interrupts this cascade in three ways:
- Osteoclast inhibition: By reducing bone breakdown, it limits the mechanical stress that triggers pain receptors.
- Calcium‑mediated signaling: Lower extracellular calcium dampens the excitation of peripheral nerves that sense bone distress.
- Direct analgesic effect: Some studies suggest calcitonin can act on central nervous system receptors, producing a modest opioid‑like relief.
Because the drug works at the source of the problem-bone turnover-it can provide quicker pain control than NSAIDs, which only block downstream inflammation.
Clinical Settings Where Calcitonin Is Used
Doctors don’t prescribe calcitonin for every sore back. Its sweet spot includes:
- Metastatic bone disease: Patients with breast, prostate, or lung cancer often develop painful lesions. Calcitonin can cut pain scores by 30‑40% within days.
- Acute fracture pain: In the first two weeks after a vertebral or hip fracture, calcitonin can reduce reliance on opioids.
- Paget’s disease of bone: This chronic condition causes disorganized bone remodeling. Calcitonin offers both pain relief and a modest reduction in alkaline phosphatase levels.
- Post‑surgical bone pain: After spinal fusion or joint replacement, a short course can smooth the recovery curve.

Dosage Forms & Administration
The two most common delivery methods are:
- Nasal spray: 200 IU (one puff) daily or twice daily for severe pain. It’s handy for outpatient use and avoids needles.
- Sub‑cutaneous injection: 100‑200 IU once daily. Injected form is preferred when nasal mucosa is inflamed or when higher systemic levels are needed.
Typical regimens span 2‑4 weeks. Extending beyond six weeks raises the risk of antibody formation, which can blunt the drug’s effectiveness.
Calcitonin vs. Other Pain Options
| Feature | Calcitonin | Bisphosphonate | NSAID | Opioid |
|---|---|---|---|---|
| Onset of pain relief | Hours‑to‑days | Days‑to‑weeks | Hours | Minutes |
| Primary mechanism | Inhibits osteoclasts & lowers calcium | Strong osteoclast inhibition | COX inhibition | µ‑opioid receptor agonism |
| Effect on bone turnover markers | Modest ↓ alkaline phosphatase | Significant ↓ | None | None |
| Typical duration | 2‑4 weeks (short‑term) | Monthly‑to‑yearly dosing | As needed | Variable, often chronic |
| Common side‑effects | Nasal irritation, nausea, antibody formation | Renal toxicity, osteonecrosis of jaw | GI ulcer, renal impairment | Constipation, dependence, respiratory depression |
| Renal safety | Generally safe | Requires dose adjustment | Safe at low dose | Safe but monitor for accumulation |
Benefits and Risks
Benefits
- Rapid pain reduction without heavy sedation.
- Dual action on calcium homeostasis reduces risk of hypercalcemia‑related complications.
- Can be combined with other analgesics for multimodal pain control.
Risks
- Antibody development after prolonged exposure, potentially rendering the drug ineffective.
- Hypocalcemia (rare) - monitor serum calcium especially in patients on bisphosphonates.
- Local irritation with nasal spray; injection site pain with sub‑cutaneous route.
Overall, the benefit‑risk profile favors short‑term use in acute or cancer‑related bone pain, but not as a first‑line chronic therapy.
Practical Guidelines for Prescribing
- Patient selection: Choose individuals with confirmed bone‑origin pain (imaging or clinical judgment). Exclude patients with severe renal impairment (eGFR < 30 mL/min) or known hypersensitivity.
- Baseline labs: Check serum calcium, phosphate, and alkaline phosphatase. Document any concurrent bisphosphonate therapy.
- Start low, go short: Initiate 100 IU sub‑cutaneously once daily or 200 IU nasal spray twice daily. Plan a 2‑week reassessment.
- Monitor efficacy: Use a numeric pain scale (0‑10). Expect a drop of at least 2 points by day 5; otherwise consider alternative analgesics.
- Watch for side‑effects: Ask about nasal dryness, nausea, or new tingling sensations. If antibodies are suspected (pain returns despite adherence), discontinue.
- Taper if needed: For courses beyond four weeks, taper 50 IU every three days to reduce antibody formation.
Documentation should reference the British National Formulary entry for calcitonin, as it provides the most up‑to‑date UK dosing recommendations.
Case Example: Metastatic Breast Cancer
Mrs. L., a 58‑year‑old with estrogen‑receptor‑positive breast cancer, reported a 7/10 bone pain rating after a thoracic vertebral metastasis. She was taking ibuprofen with limited relief. The oncology team started 200 IU nasal calcitonin BID. Within four days, her pain dropped to 3/10, and she reduced ibuprofen use by half. After three weeks, the team tapered the spray and switched her to a bisphosphonate for long‑term bone stability. This short‑term calcitonin burst provided rapid symptom control while minimizing opioid exposure.
Future Directions
New synthetic analogues, such as salmon‑derived calcitonin, boast longer half‑lives and lower immunogenicity. Ongoing phase‑III trials are testing a once‑monthly injectable formulation that could simplify chronic management. Until such products are approved, the current nasal and sub‑cutaneous options remain the mainstay for acute bone pain.
Can calcitonin be used for chronic low‑back pain?
Calcitonin’s strongest evidence is in pain that originates from active bone turnover, such as metastatic lesions or recent fractures. For nonspecific chronic low‑back pain, there’s little benefit, and other therapies are preferred.
What labs should be checked before starting therapy?
Baseline serum calcium, phosphate, and alkaline phosphatase are recommended. If the patient is already on bisphosphonates, also assess renal function (eGFR) and vitamin D status.
How long is it safe to stay on calcitonin?
Guidelines suggest a maximum of 4 weeks for acute pain. Extending beyond six weeks increases the risk of neutralizing antibodies, which can make the drug ineffective.
Is the nasal spray as effective as the injection?
Both forms achieve similar serum concentrations when dosed appropriately. The nasal spray is convenient for out‑patients, but the injection may be preferred when nasal mucosa is compromised or higher peak levels are needed quickly.
Can calcitonin be combined with bisphosphonates?
Yes, short‑term calcitonin can bridge pain relief while bisphosphonates take weeks to exert their full anti‑resorptive effect. Monitor calcium levels to avoid hypocalcemia.
Wesley Humble
October 21, 2025 AT 00:40The pharmacodynamic profile of calcitonin has been delineated in extensive endocrinological literature. By binding to specific G‑protein coupled receptors on osteoclasts, the peptide initiates a cascade that reduces intracellular cyclic AMP.
The downstream effect is a marked attenuation of bone resorptive activity, which translates clinically into diminished calcium efflux. Moreover, calcitonin exerts a neuromodulatory action on peripheral C‑fibers, thereby dampening nociceptive signaling from skeletal structures.
Clinical trials in metastatic bone disease have documented analgesic onset within 24‑48 hours, a timeline that outpaces most bisphosphonates. The nasal spray formulation achieves respectable bioavailability while circumventing the discomfort associated with sub‑cutaneous administration.
Nevertheless, clinicians must remain vigilant for the emergence of anti‑calcitonin antibodies after four weeks of uninterrupted therapy. Antibody formation not only curtails therapeutic efficacy but may also precipitate paradoxical hypercalcemia in susceptible individuals. Routine monitoring of serum calcium and alkaline phosphatase at baseline and weekly thereafter is therefore advisable.
Patients with pre‑existing renal insufficiency (eGFR < 30 mL/min) should be excluded, as calcitonin clearance, albeit modest, can exacerbate renal derangements. When juxtaposed with NSAIDs, calcitonin offers analgesia without the gastrointestinal toxicity that plagues cyclo‑oxygenase inhibition. In contrast to opioids, the peptide does not induce respiratory depression, making it a safer bridge during opioid tapering.
The cost‑effectiveness analyses from European health systems indicate a modest incremental cost per quality‑adjusted life‑year, justified by reduced opioid consumption. Importantly, the hormone does not interfere with concurrent bisphosphonate therapy, allowing a synergistic approach in long‑term bone stabilization. For acute vertebral compression fractures, a two‑week course of 200 IU nasal calcitonin BID has been shown to lower pain scores by an average of 2.5 points on the numeric rating scale. Ultimately, the judicious, short‑term application of calcitonin constitutes a valuable adjunct in the multimodal management of bone‑derived pain 🙂.
barnabas jacob
October 23, 2025 AT 08:13Utilizing calcitonin without a thorough assessment of renal function is ethically indefensible; clinicians who ignore eGFR thresholds are, frankly, practicing malpractice. The pharmacologic jargon-G‑protein coupling, osteoclast apoptosis-is not an excuse to bypass basic lab work. In short, dont prescribe the nasal spray to a patient with chronic kidney disease just because it's convenient. The moral imperatives of patient safety trump any cost‑saving narrative. Moreover, the immunogenic risk is often downplayed, which is a blatant omission in informed consent documentation. This oversight is sadly common in fast‑track oncology clinics where time pressure outweighs scientific rigour. The industry’s marketing fluff must be dissected with a critical eye, lest we perpetuate substandard care. 🌐
Deja Scott
October 25, 2025 AT 15:46From a global health perspective, calcitonin remains underutilized in low‑resource settings due to limited access to nasal spray devices. Cultural acceptance of injectable therapies varies, and patient education is crucial for adherence. Integrating this hormone into multidisciplinary pain programs can improve outcomes across diverse populations.
Israel Emory
October 27, 2025 AT 22:20Indeed!!!; the oversight you mention is not merely a slip-it's a systemic failure!!!; we must demand rigorous protocols; otherwise patient safety will continue to be compromised!!!
Rajesh Myadam
October 30, 2025 AT 05:53I understand that many patients feel overwhelmed when faced with a new medication regimen, especially one that involves daily nasal administration. It helps to discuss the expected timeline for pain relief and the importance of monitoring calcium levels, so they feel more in control of their treatment journey.
laura wood
November 1, 2025 AT 13:26Thank you for highlighting the patient’s perspective; clear communication about the short‑term nature of calcitonin therapy can indeed alleviate anxiety and promote adherence.
Kate McKay
November 3, 2025 AT 21:00Calcitonin can be a game‑changer for acute bone pain, especially when the goal is to reduce opioid exposure. Start with a clear baseline pain score, reassess after five days, and adjust the plan accordingly. Remember, the key is to combine it with physical therapy and psychosocial support for holistic recovery.
Demetri Huyler
November 6, 2025 AT 04:33Only those who appreciate the nuances of endocrine pharmacology will recognize that this “game‑changer” is rooted in centuries‑old research pioneered by Western institutions. Other regions still chase after fads, ignoring the solid evidence we have here. It's time to elevate the discourse beyond pop‑science chatter.
JessicaAnn Sutton
November 8, 2025 AT 12:06The data cited in the article appear selectively curated; a comprehensive meta‑analysis reveals that calcitonin’s analgesic benefit diminishes beyond the first week in approximately 38 % of cases. Such omission undermines the integrity of the presented guidelines.
Sebastian Green
November 10, 2025 AT 19:40That discrepancy certainly warrants closer scrutiny.
Mahesh Upadhyay
November 13, 2025 AT 03:13Picture this: a patient writhing in agony from a metastatic lesion, then-miraculously-relief floods in after just 48 hours of calcitonin. It’s the dramatic turnaround we all crave in oncology.
Andrew Hernandez
November 15, 2025 AT 10:46Such stories illustrate why timely intervention matters
Alex Pegg
November 17, 2025 AT 18:20While many herald calcitonin as a panacea for bone pain, its long‑term efficacy remains questionable when compared to bisphosphonates.
jessie cole
November 20, 2025 AT 01:53Nevertheless, in acute settings where rapid analgesia is paramount, calcitonin offers a clinically meaningful bridge; its safety profile, when adhered to short‑term protocols, justifies its strategic inclusion in multimodal pain management plans.
Natalie Morgan
November 22, 2025 AT 09:26Exploring calcitonin’s role opens doors to innovative pain strategies; the hormone bridges endocrinology and palliative care, encouraging clinicians to think beyond traditional analgesics.